
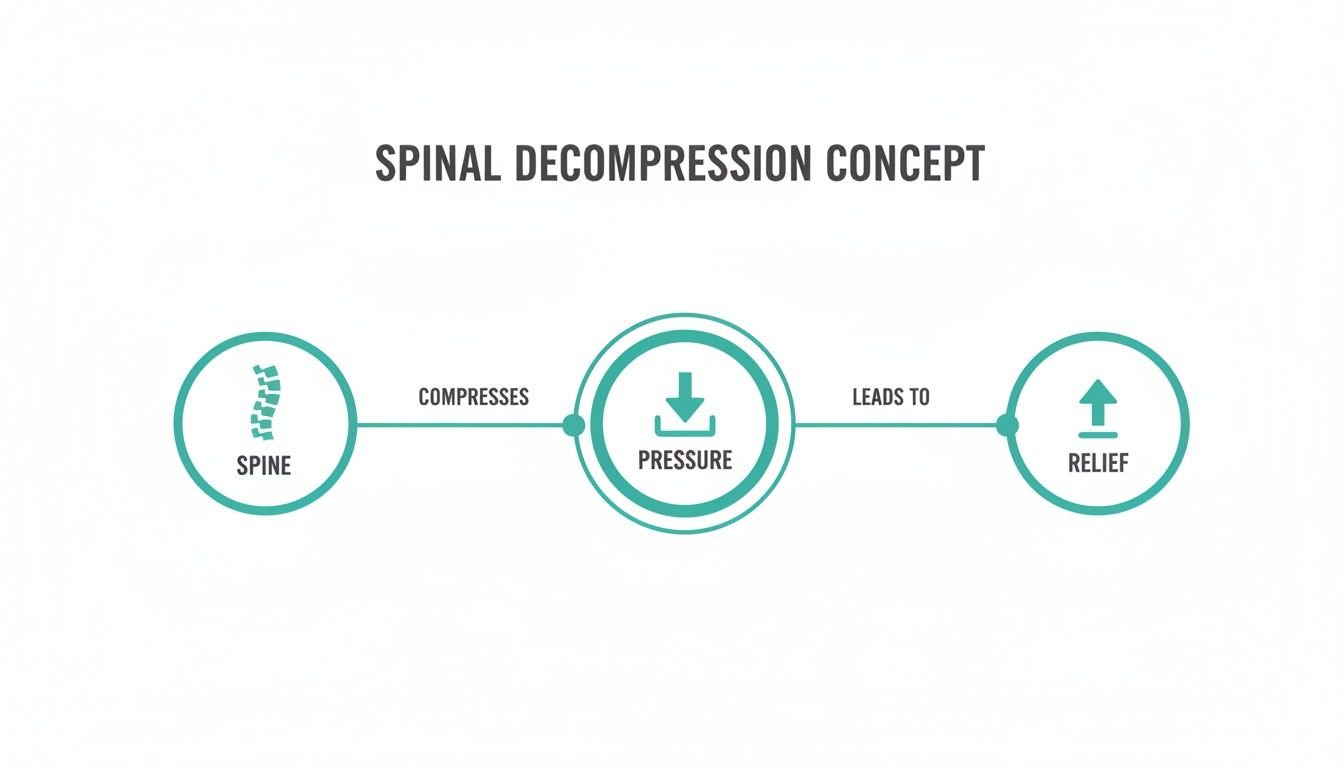
Spinal decompression is a non-surgical therapy that gently stretches the spine using a specific, motorized table. The goal is simple but effective: relieve pressure on your spinal discs and nerves to ease chronic pain in the back, neck, or legs, especially pain from conditions like herniated discs or sciatica.
Let's think of your spine like a stack of doughnuts (your vertebrae) with jelly-filled centers (your discs). Through daily life, injury, or just getting older, those jelly-filled discs can get squashed, causing the jelly to bulge out and press on nearby nerves. That pressure is what causes the shooting pain, numbness, or tingling that can make life miserable.
Spinal decompression targets this problem directly. It’s designed to gently and precisely create more space between the vertebrae. As this happens, it creates a subtle negative pressure, almost like a tiny vacuum, inside the damaged disc.
This vacuum effect, technically called negative intradiscal pressure, is the secret sauce. It helps coax the bulging or herniated disc material back into its rightful place, getting it off the pinched nerve.
But the process doesn't stop there. Relieving the immediate pressure is only half the battle; the real magic is in kickstarting the healing process.
Imagine a dried-out kitchen sponge. If you squeeze it, it can't soak up any water. But as soon as you let go, it immediately draws in liquid. A compressed spinal disc is a lot like that. Decompression gives it the breathing room it needs to pull in vital resources.
This allows the disc to absorb:
This flood of resources helps your body heal the disc from the inside out. It's not just a quick fix for the pain; it's a method aimed at restoring the long-term health and function of the spine.
This focus on non-invasive, lasting relief is why spinal decompression is becoming a go-to option. In fact, the market for these devices was valued at around $3.98 billion in 2023 and is expected to keep growing as more people look for alternatives to surgery. You can discover more insights about this growing market and see how it's changing pain management. For many, it's a powerful way to find lasting relief without going under the knife.
So, how does spinal decompression actually work? To really get it, we need to look past the idea of a simple stretch and dig into the clever science happening inside your spine. The therapy’s magic lies in its ability to create the perfect environment for damaged discs to pull back in and heal on their own. It all boils down to a key concept called negative intradiscal pressure.
Picture your spinal discs as little jelly-filled donuts, or cushions, between your vertebrae. When a disc is herniated or bulging, the pressure inside is high, pushing that jelly-like material outward and often right onto a nerve. The whole point of spinal decompression is to reverse that pressure by gently, and very precisely, pulling the vertebrae apart.
This isn't just a random tug-of-war. The pulling force is applied in a specific, logarithmic way that creates a vacuum effect right inside the disc. This vacuum is the negative intradiscal pressure, and it’s what sets the stage for healing.
Once that negative pressure is created, a couple of crucial things start to happen. First, it helps suck the bulging or herniated disc material back to where it belongs. Think of using a suction cup to pull a small dent out of a car door—the vacuum pulls the metal back into place. It’s a similar idea here; the vacuum inside the disc coaxes that protruding material back into the center, taking the pressure off the pinched nerve.
This is a huge reason why people often feel relief from radiating pain like sciatica so quickly. We're addressing the mechanical root of the problem, which helps stop the nerve irritation causing that pain, numbness, or tingling down your legs or arms.
This flowchart shows the simple but powerful idea behind the therapy: apply a controlled force, relieve the pressure, and allow healing to start.
It’s all about interrupting that cycle of compression and pain to create an opening for real recovery. This targeted approach is what makes it so different from more general treatments.
Your body is pretty smart. It has a built-in defense system called the muscle-guarding reflex. When your spine feels a sudden or aggressive stretch, the big muscles around it instinctively clamp down to protect you from injury. This is actually a major problem for older, traditional traction methods, which often trigger this reflex and end up fighting against the very muscles they're trying to stretch.
Modern spinal decompression, however, is designed to be much more clever.
The computer-controlled system applies tension so slowly and gently that it essentially flies under the radar of your body’s protective sensors. By ramping the force up and down in precise, oscillating cycles, the therapy bypasses that muscle-guarding reflex entirely.
This allows us to achieve a much deeper and more effective separation of the vertebrae—something basic traction just can't do. It's the key to creating the significant negative pressure needed for true disc healing.
While older traction methods have their place, understanding their limitations is key. The table below breaks down the major differences.
| Feature | Spinal Decompression Therapy | Traditional Traction |
|---|---|---|
| Mechanism | Creates negative intradiscal pressure using computer-controlled, logarithmic pull patterns. | Applies a static or intermittent linear pull to the spine. |
| Muscle Guarding | Designed to bypass the body's muscle-guarding reflex for a deeper, more targeted effect. | Often triggers muscle guarding, which can limit the effectiveness of the stretch. |
| Technology | Utilizes advanced computer systems to monitor and adjust forces in real-time. | A simpler mechanical device with limited feedback or adjustment capabilities. |
| Patient Experience | Generally comfortable and relaxing, as the forces are applied gently and precisely. | Can sometimes be uncomfortable due to the more aggressive, sustained pulling force. |
| Targeting | Can isolate specific spinal segments (e.g., L4-L5) for focused treatment. | Pulls on the entire spine or a large region, making it less specific. |
Ultimately, this intelligent approach is what truly separates modern decompression from its predecessors. If you want to dive deeper into other traction-based therapies, you can explore our guide on what is intersegmental traction.
The second major benefit of creating that negative pressure is how it kickstarts the healing process. A healthy spinal disc is mostly water—about 80%, in fact. But when a disc gets compressed or damaged, it starts to dry out, becoming brittle and losing its ability to absorb shock.
Think of a dried-out kitchen sponge. If you put a heavy plate on it, it can't soak up any water. But the second you lift that plate, the sponge expands and eagerly pulls in any nearby liquid.
Spinal decompression does the exact same thing for your discs. By creating that space and vacuum effect, it allows a flood of healing resources to rush back into the disc. This includes:
This natural process is called imbibition, and it's how the disc revitalizes itself from the inside out. This isn't just about temporary relief; it’s about helping the disc return to a healthier, more resilient state. It's a proactive approach focused on restoring function, not just chasing symptoms.
Figuring out if a new treatment is right for you can be a lot to take in. When it comes to spinal decompression, however, the process is pretty straightforward. It’s a targeted, non-surgical therapy that works wonders for very specific back and neck problems, but it’s definitely not a magic bullet for every type of pain.
The key is understanding what it does best. Decompression therapy is designed for people whose pain is caused by mechanical pressure on their spinal discs and nerves. If the problem is compression, creating space just makes sense.
We’ve seen incredible results with spinal decompression for a handful of common, and often debilitating, conditions. By gently and precisely separating the vertebrae, we can get right to the source of the problem.
Here are the issues where this therapy really shines:
Knowing who shouldn't do this therapy is just as important as knowing who should. While the pulling force is gentle, it can be risky for people with certain health issues that affect the stability of their spine. That's why a completely honest and thorough medical history is so vital for your safety.
A full evaluation before starting any treatment is non-negotiable. We have to rule out any contraindications to protect you from harm and make sure we’re only using this therapy where it can be both safe and effective.
Generally, spinal decompression is not the right move for people with any of the following:
The fact that this therapy is becoming more common speaks volumes about how well it works for the right person. The market for spinal decompression devices is already huge—estimated between USD 650 million and over a billion dollars globally—and it's expected to keep growing. This isn't some fringe treatment; it's a core part of modern pain management.
In the end, the only way to know for sure if you’re a candidate is to come in for a detailed consultation. We’ll need to look at your imaging (like an MRI), understand your exact diagnosis, and talk through your history. From there, we can build a plan that safely gets to the root cause of your pain.
Starting any new treatment can feel a little intimidating, but we want to pull back the curtain on spinal decompression therapy so you know exactly what’s involved. The entire process is designed to be a comfortable, relaxing, and cumulative healing experience. Think of it this way: each session builds on the progress of the last, gradually working to relieve pain and restore function right at the source.
From the moment you walk in for your first appointment, we'll guide you through everything. Our goal isn’t just to treat your condition, but to make the healing process itself a positive and reassuring part of your recovery.

I know the idea of being "stretched" by a machine might sound a bit intense, but the reality is the exact opposite. The experience is so gentle and controlled that many of our patients find it incredibly relaxing. It's not uncommon for people to doze off during treatment.
Here’s a simple breakdown of what a typical appointment looks like:
We monitor the entire process from start to finish. The real objective here is to create a state of deep relaxation, which allows your spine to accept the therapy and kickstart its natural healing process without any resistance.
It's really important to understand that spinal decompression isn't a one-and-done fix. While some people feel a measure of relief after just a handful of sessions, the real, lasting benefits are built up over time. The therapy works by gradually rehydrating the disc, helping retract bulging material, and stimulating long-term tissue repair.
Think of it like watering a neglected plant. One good watering helps, but it’s the consistent care over several weeks that truly brings it back to vibrant health. Spinal decompression works on the same principle, delivering steady, gentle therapy to foster deep healing.
A standard treatment plan involves a series of sessions scheduled over several weeks. While every plan is customized, a common protocol might look something like this:
This structured approach gives your discs the consistent therapeutic input they need to heal correctly and, just as importantly, for the results to stick around long-term.
At Bonesetters, we know from experience that the best outcomes happen when we treat the body as a whole system. To boost the effects of spinal decompression and speed up your recovery, we almost always weave supportive therapies into your treatment plan. These complementary treatments work in concert to reduce inflammation, improve your mobility, and strengthen the muscles that support your spine.
Your personalized plan may include a combination of:
By combining these methods, we’re able to address your condition from multiple angles. This integrated strategy is the key to achieving significant, lasting relief and getting you back to living your life to the fullest.
When you’re dealing with chronic pain, you really only care about one thing: does this treatment actually work? For spinal decompression therapy, the answer is a resounding "yes," backed by a growing body of clinical research and, just as importantly, countless real-world success stories. We're not talking about wishful thinking here; we're talking about measurable changes in your body that lead to genuine pain relief.
Let’s skip the dense medical jargon and get straight to what the research means for you. Study after study shows significant improvement for patients who are good candidates for this therapy. And we don't mean minor tweaks—we're talking about major drops in pain levels and the ability to get back to daily activities that pain had made impossible.
The most powerful evidence comes from looking at what’s happening inside your spine. Before-and-after MRIs often show clear, positive changes. Researchers have documented visible increases in the height of worn-out discs, a direct sign that they are rehydrating and beginning to heal.
This internal healing is what you feel on the outside. In the clinic, we consistently see a few key outcomes:
One study really drove home the impact. Patients who finished 20 sessions of decompression therapy reported an 80% reduction in pain and a 50% improvement in their disability scores. Even better, their follow-up MRIs revealed an average disc height increase of about 1.0–1.6 mm. That might not sound like much, but in the tight quarters of the spine, it’s a huge deal. You can dig into the details of these disc lesion study findings for a closer look at the data.
While the evidence is incredibly positive, it's vital to have realistic expectations. Spinal decompression is a powerful tool, but it's not a magic wand. Your personal results will hinge on a few key factors.
The success of spinal decompression therapy is deeply connected to a precise diagnosis and unwavering patient commitment. It's a partnership between the practitioner's expertise and the patient's dedication to completing the full healing process.
Here’s what can influence your outcome:
At Bonesetters, our evidence-based approach is built to give you the best possible shot at success. We start with a meticulous diagnostic process to confirm you’re a great candidate. From there, we map out a personalized treatment plan that targets your specific issue, creating the strongest foundation for significant, lasting relief.
When you're dealing with back pain, two questions inevitably come up: "What's this going to cost me?" and "What else can I try?" Let's break down where spinal decompression fits into the picture, both financially and when compared to other common treatments. It’s all about helping you make a smart, informed choice for your health.
The cost of spinal decompression can vary, but we believe in being upfront about it. The price is usually set per session, and a complete course of treatment will involve a series of appointments over several weeks.
So, what are we talking about in terms of numbers? A single session typically runs from $75 to $200. A full treatment plan, designed to get you lasting results, often lands somewhere between $1,500 and $4,000. While that might sound like a lot at first glance, it’s important to remember that it's often a fraction of the cost of going under the knife.
Insurance coverage can be a bit hit-or-miss. Some carriers are fully on board, while others still view it as an emerging therapy. The best first step is always to call your provider and ask about your specific benefits. We're here to help by giving you the right billing codes and paperwork you need to figure out what’s covered.
Investing in a comprehensive, non-surgical treatment like spinal decompression is not just about managing pain today. It's about restoring function and preventing the need for far more invasive and costly procedures down the road.
Think of back pain treatments as a spectrum. On one end, you have conservative care, and on the other, you have major surgery. Spinal decompression sits right in that powerful middle ground, offering a solution when simpler methods aren't enough.
Let's see how it compares to the alternatives:
Physical Therapy and Chiropractic Adjustments: These are often the first line of defense. PT is fantastic for building up the muscles that support your spine, and adjustments are great for restoring joint movement. Decompression takes a different, more focused approach by directly targeting the disc itself, creating that crucial negative pressure to kickstart the healing process. In fact, it often works best when used alongside these other therapies.
Epidural Steroid Injections: Injections can be a game-changer for short-term pain relief by flooding an irritated nerve with anti-inflammatory medicine. The catch? They don't fix the source of the problem—the squashed disc. Decompression is all about addressing that root mechanical issue for relief that actually lasts.
Surgical Options (Discectomy or Laminectomy): Surgery is, and should be, the last resort. These procedures involve physically removing parts of the disc or bone to free up a nerve. They can be effective, but they also come with serious risks, a lengthy recovery, and a hefty price tag. Spinal decompression gives you a chance to achieve a similar outcome without the scalpel and downtime.
For anyone looking to sidestep surgery, exploring a non-surgical disc herniation treatment like this is a very logical next step. It beautifully bridges the gap between therapies that offer temporary relief and an operation you may not need, giving your body a real chance to heal itself.
It’s completely normal to have a few questions running through your mind before trying a new therapy, even after you understand the basics. To help you feel confident in your decision, we've put together some straight-to-the-point answers to the questions we hear most often. Think of this as the final piece of the puzzle in figuring out if this is the right path for you.
Absolutely not. The entire experience is designed to be gentle and comfortable. You’ll be securely positioned on the table, and the computer-controlled system applies a slow, gradual pulling force.
Most people describe the sensation as a mild, welcome stretch. In fact, it’s so relaxing that it’s not uncommon for patients to fall asleep during the session.
This is a marathon, not a sprint. While some people notice a bit of relief right away, the real, lasting benefits of spinal decompression build up over time. It's a lot like physical therapy in that sense—consistency is key.
You can typically expect to see significant, durable improvement over the full treatment plan, which usually runs for about four to six weeks. How quickly you respond really depends on the severity of your condition and sticking to the schedule.
That's a great question, but no, they are fundamentally different. An inversion table uses gravity and your own body weight to create a static stretch. The problem is, this can sometimes cause your back muscles to tense up in response (a "muscle guarding" reflex), which fights against the stretch.
Spinal decompression, on the other hand, uses a sophisticated, computer-guided system. It applies a precise, intermittent pull to a specific spinal segment, intelligently working to bypass that muscle guarding reflex. This allows for a much deeper and more targeted decompression of the disc.
For the right candidate, the success rate is impressively high. Many studies and clinics report success rates somewhere between 70% and 90%.
"Success" here usually means a major reduction in pain and a real improvement in your ability to get back to daily activities. Of course, hitting these numbers depends entirely on getting an accurate diagnosis from the start and the patient seeing the full treatment plan through to the end.
At Bonesetters, our evidence-based protocols are built to give you the best possible shot at lasting relief. If you're ready to explore a non-surgical solution to your pain, discover our personalized approach to spinal decompression by visiting us at https://bonesetters.org.