When you get the news that you have a "slipped disc," it's easy to feel a jolt of panic. The word itself sounds severe, and for many, the immediate fear is surgery. But let me be the first to tell you what I've seen in my practice for years: for the vast majority of people, slipped disc recovery without surgery isn't just a hopeful idea—it's the most common and successful path forward. Your body is an incredible healing machine, and when guided by the right conservative care, it can often resolve the issue on its own.

The moment you hear "herniated disc," it's natural for your mind to jump straight to the operating table. It's a common fear, but it’s one that’s largely fueled by outdated thinking about back pain. The reality? Surgery is rarely the first answer. This entire guide is built on the principle that effective, non-invasive treatments should be the first line of defense—the gold standard for getting to the root cause of your pain.
Let's talk about a real-world scenario I see all the time. Think of someone like Sarah, a 45-year-old who spends her days at a desk. After a weekend of intense gardening, she suddenly felt a sharp, shooting pain down her right leg. An MRI confirmed a lumbar disc herniation. Her initial panic was real, but it quickly turned into a proactive mindset once she understood that her body was already working hard to heal itself.
This isn't just wishful thinking; it's backed by solid science. Before we go any further, let's look at the numbers. They offer a lot of reassurance.
| Statistic | Success Rate / Finding |
|---|---|
| Initial Improvement | Up to 90% of patients improve without surgery within 6 weeks. |
| Surgery Rate | Only 10% of patients with acute lumbar herniations required surgery in the first six weeks. |
| Spontaneous Regression | A significant number of herniated discs shrink or disappear on their own over time. |
These figures, drawn from research like a key study in The Spine Journal, paint a clear picture. The study followed 147 patients and found that an overwhelming majority got better without going under the knife. You can discover more insights about these non-surgical outcomes.
What this really means is that your body has an incredible, built-in capacity for repair. The entire goal of conservative care is simply to create the perfect environment for that natural healing process to unfold.
So, what does that "perfect environment" look like? Effective recovery isn't about finding one magic bullet. It's about a strategic, layered approach where different therapies work together to reduce your pain, get you moving properly again, and prevent this from happening in the future.
Your journey back to health will focus on a few core principles:
By focusing on these pillars, you empower your body's own healing mechanisms. A successful non-surgical recovery isn't about passively waiting for the pain to go away; it's an active process of giving your body the support it needs to fix the problem at its source.
When a doctor says you have a "slipped disc," it sounds terrifying. You picture a part of your spine literally slipping out of place, but that’s not what’s happening at all. Your discs are actually anchored quite securely between your spinal bones (the vertebrae).
So what's really going on? Think of your spinal discs as little jelly donuts. They have a tough, chewy outer ring (the annulus fibrosus) and a squishy, gel-like center (the nucleus pulposus). These "donuts" sit between your vertebrae, acting as perfect shock absorbers and letting your spine move freely.
A "slipped disc" is just a problem with this little donut. When the tough outer ring gets damaged, the jelly center can start to push out, creating all sorts of trouble.
Your doctor might use a couple of different terms, and knowing the difference is key to understanding your situation. They aren't the same thing, though people often use them interchangeably.
Disc Bulge: This is an early-stage issue. Imagine squashing the jelly donut just enough that it pooches out around the edges. The outer wall is still intact, just stretched and stressed. A bulge can be completely silent, or it might be the first warning sign that something's not right.
Disc Herniation: This is more serious. A tear has actually formed in the tough outer wall, and the jelly-like center is leaking out. This escaped gel is what can press on the incredibly sensitive nerves running along your spine.
Professionals almost always use the term herniated disc because it’s much more accurate. It’s the pressure from this herniated material that triggers those classic, often debilitating, symptoms.
Disc injuries rarely happen out of the blue. They're usually the result of one big, sudden event or, far more often, the slow accumulation of stress over years. Figuring out the "why" is a huge part of making sure it doesn't happen again.
Here are the usual suspects:
Sudden Trauma: This is the one you remember. Lifting something heavy with bad form, a sudden awkward twist, a fall, or a car accident can create enough force to rupture the disc in an instant.
Repetitive Strain: This is the silent culprit. Years of poor posture at a desk, repeated bending and twisting at work, or even just not moving enough can slowly weaken the disc fibers. Eventually, something as simple as a cough or a sneeze can be the final straw.
Age-Related Changes: It’s a fact of life. As we get older, our discs lose water and become less flexible—a process called disc degeneration. This makes them more prone to tearing.
That pain you're feeling is a direct signal. Sciatica, for example, isn't a condition; it's a symptom. That sharp, shooting pain down your leg is a nerve screaming that it's being pinched or irritated by that herniated disc material in your lower back.
Once you connect the dots between the anatomy, the cause, and your symptoms, the diagnosis becomes much less scary. You can see it for what it is—a mechanical problem. And that's the first step toward fixing it without surgery.
When you’re facing a slipped disc, the goal isn't to find a single magic bullet. Real, lasting recovery comes from a multi-pronged approach where several powerful therapies work together. Think of it as building a strong foundation for healing. Each part of the plan addresses a different piece of the puzzle, and when combined, they give your body the best possible chance to repair itself without surgery.
And here’s the most important thing to remember: your body is built to heal. The odds are actually in your favor. A staggering 80-90% of herniated disc cases get better on their own with the right conservative care. This isn't just wishful thinking; it's what we see in the clinic every day, and it's backed by research. Orlando Health confirms that most disc issues resolve long before surgery is even on the table. This high success rate for non-surgical recovery should give you a lot of confidence as we dive into the therapies that make it happen.
At its core, a disc injury is often a mechanical problem. Something in your spine isn't moving the way it should, and that puts a ton of stress on your discs. Advanced chiropractic care gets to the root of this by restoring healthy, precise motion to your spinal joints.
This isn't about aggressive "cracking." We use gentle, computer-guided tools like the PulStar system to deliver targeted impulses to the exact vertebrae that are causing the problem. It’s a subtle but powerful way to coax the spine back into proper alignment. Doing this helps to:
By addressing the faulty mechanics first, we create a stable base for all the other treatments to work their magic.
Imagine if you could gently create space around that injured disc, giving it room to breathe and heal. That's exactly what non-surgical spinal decompression does. It’s a game-changer in modern disc recovery because it directly counteracts the very compressive forces that caused the injury in the first place.
Here’s how it works: you lie comfortably on a specialized, computer-controlled table that applies a very gentle, calculated pull to your spine. This action creates negative pressure—a vacuum effect—inside the damaged disc.
A Simple Analogy: Think about trying to suck a drop of spilled jelly back into a donut. Spinal decompression creates a similar vacuum that helps gently draw the herniated material back towards the center of the disc and, most importantly, away from that pinched nerve.
This process delivers two incredible benefits:
While decompression is fixing the mechanical problem, Class IV Cold Laser Therapy gets to work on the biological side of things. A huge part of the pain from a slipped disc comes from inflammation. Getting that under control is critical.
This advanced therapy uses specific wavelengths of light that penetrate deep into your tissues. It’s not a "hot" laser; it's a "cold" one that triggers a process called photobiomodulation. In plain English, it gives a massive energy boost to your cells' mitochondria—their little power factories. This sets off a cascade of healing effects:
For anyone with a slipped disc, this translates to less pain, less swelling, and a much faster path to recovery.
Once we've got the pain and inflammation dialed down, the final pillar is building strength and stability so this never happens again. This is where targeted physical therapy comes in. We’re not talking about generic gym workouts; we’re talking about a specific set of exercises prescribed just for your injury.
The focus is almost always on the deep core muscles—the transverse abdominis, multifidus, and pelvic floor. These muscles form a natural corset that supports your spine and takes the load off your discs. The right exercises will help you build a stable core without putting your spine through risky movements. For example, many of our patients get incredible results with highly structured protocols like the McKenzie Method. You can learn more in our guide on the McKenzie Method for sciatica and disc pain.
Together, these pillars—chiropractic, decompression, laser therapy, and targeted exercise—create a comprehensive framework for healing. They don’t just cover up the symptoms; they work in sync to fix the underlying problems, paving the way for a full recovery without going under the knife.
When you're dealing with a slipped disc, the road to recovery can feel long and uncertain. Let's be honest, it's easy to get discouraged.One of the most important things I tell my patients is that knowing what’s ahead is half the battle. Recovery isn't a straight line; it's a process with distinct phases. Understanding these stages helps you stay motivated and recognize the small wins along the way.
Think of it as a roadmap. We start by putting out the fire, then we carefully rebuild the foundation, and finally, we fortify the structure to prevent future problems.
This visual gives you a great overview of the journey from initial pain to long-term strength.
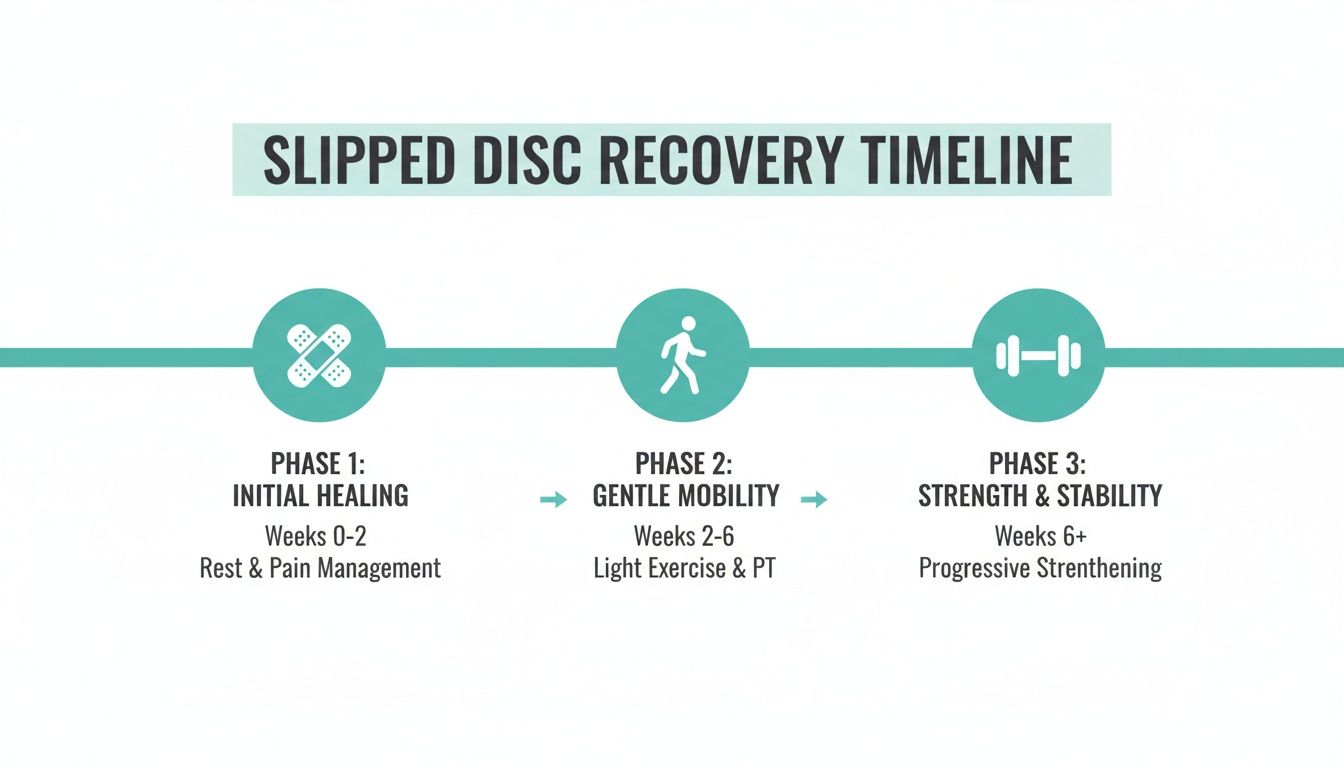
As you can see, healing is a progression. It all starts with calming the acute issue before we can methodically move toward restoring full, robust function.
The first month is all about damage control. The goal here is simple: reduce that intense, searing pain and calm the inflammation that's screaming at your nerves. This is absolutely not the time to be a hero and push through the pain.
Your focus should be on gentle, controlled movements and consistent conservative care. This is where chiropractic adjustments and spinal decompression can be game-changers, helping to take direct pressure off the pinched nerve. A tool like a spinal decompression chair works by creating negative pressure inside the disc, which can help the herniated material retract and pull in the nutrients needed for healing.
What to Do:
What to Avoid:
By the end of this phase, the sharp, electric-shock-like pain should be noticeably better. You'll likely still have a dull ache, but that debilitating, stop-you-in-your-tracks pain should start to fade.
Now that the fire is mostly out, the next two months are dedicated to rebuilding. Your body is busy laying down new, stronger collagen fibers to repair the disc. Our job is to support that process with the right kind of movement.
This is where we shift from passive pain relief to active strengthening. Targeted core stabilization exercises become your new best friend. We're not talking about crunches; we're retraining the deep, stabilizing muscles like the transverse abdominis and multifidus to act as a natural corset for your spine.
A Word of Caution: This is the phase where people get into trouble. You're feeling better, so you jump back into your old routine too fast and—BAM—you're back at square one. Progress has to be slow and steady.
During these weeks, you should find you can sit a bit longer and walk farther with less trouble. Your overall mobility will improve, and you’ll start to trust your body again.
Once you’ve built a stable core and relearned proper movement patterns, it’s time to bulletproof your back for the long haul. The goal now is to build so much strength and resilience that the risk of this happening again becomes incredibly small.
This means progressing your core work, reintroducing more complex movements (like how to squat and lift with perfect form), and gradually getting back to the sports and hobbies you love. You're not just recovering; you're building a stronger, smarter body.
Your success in this phase isn't just measured by the absence of pain. It's measured by your ability to lift your groceries, play with your kids, or go for a run without a second thought.
To make it easier to see what you should (and shouldn't) be doing at each stage, here is a quick-reference guide.
This table breaks down the activities that are generally safe and beneficial during each phase of your recovery journey. Always listen to your body and consult with your healthcare provider before starting any new activity.
| Recovery Phase | Focus | Recommended Activities | Activities to Avoid |
|---|---|---|---|
| Acute Phase (Weeks 1-4) | Pain & Inflammation Control | Gentle walking (5-10 mins), positional relief, prescribed nerve glides, deep breathing exercises. | Bending, lifting, twisting (BLT), prolonged sitting, high-impact activities (running, jumping), aggressive stretching. |
| Remodeling Phase (Weeks 5-12) | Core Stability & Mobility | Longer walks (15-30 mins), swimming/water aerobics, stationary cycling, foundational core exercises (e.g., bird-dog, dead bug). | Heavy lifting, contact sports, exercises that cause sharp pain, sudden twisting motions (e.g., golf swing). |
| Strengthening Phase (3+ Months) | Functional Strength & Resilience | Bodyweight squats and lunges (with proper form), light resistance training, gradually returning to sports and hobbies. | Pushing through pain, poor lifting mechanics, neglecting core work, overtraining. |
Remember, this guide provides a general framework. Your personal timeline might be faster or slower, and that's perfectly okay. The key is consistent, patient effort.
What you do in the clinic is only half the battle. Real, lasting recovery from a slipped disc happens in the small choices you make every single day. The food you eat, the way you sleep, how you manage stress—these factors create the environment your body either needs to heal or struggles against.
Think of it like this: your treatments are the expert crew brought in to fix the problem. Your lifestyle choices are the materials they have to work with. You can't expect a solid repair with shoddy materials, and that's why these daily habits are a cornerstone of a successful slipped disc recovery without surgery.
Inflammation is the engine driving a lot of your pain. While our clinical treatments target it directly, your diet can either douse the flames or pour gasoline on them. An anti-inflammatory diet isn't just a "nice-to-have"; it's a powerful tool in your recovery kit.
The goal is to focus on whole, nutrient-dense foods that give your body what it needs to repair damaged tissue.
At the same time, you need to sideline the foods that actively promote inflammation. This means cutting way back on processed foods, sugary drinks, and refined carbs like white bread and pastries.
A simple swap can make a huge difference. Ditching a morning bagel for a bowl of oatmeal with berries and walnuts instantly flips your breakfast from pro-inflammatory to anti-inflammatory. That one change directly supports your body’s healing mission.
Did you know your spinal discs are mostly water? That’s why proper hydration is completely non-negotiable for their health. Staying hydrated keeps them plump and better able to absorb shock. It’s one of the easiest and most effective things you can do for your spine.
Just as critical is where you spend a third of your life: your bed. If your spine is twisted or unsupported all night, it's a massive roadblock to healing. A supportive mattress and the right pillow are crucial investments. After all, a key part of recovery involves finding the best mattress for back pain.
When you sleep in proper alignment, your back muscles can finally relax completely, allowing the discs to decompress and rehydrate overnight.
For many of us, our workspace is a minefield for back health. Sitting for hours, especially in a bad chair, puts a ton of pressure right on your lumbar discs.
A few simple ergonomic tweaks can provide immediate relief:
Finally, don't underestimate the power of stress. When you're stressed, your muscles—especially in your back—clench up. This adds more pressure to an already angry disc.
Bringing in some simple stress-management techniques like deep breathing, meditation, or even a gentle walk can lower that muscle tension and dial down your pain. These practices are just as vital as any physical exercise. You can explore more movement-based options in our guide to the best exercises for lower back pain relief.
Look, while this entire guide is built around the fact that most slipped discs heal without surgery, there are a few situations where you absolutely must seek immediate medical help. This isn't about fear-mongering; it's about being smart and safe.
Some symptoms are more than just pain—they're signals of a serious neurological problem that conservative care simply can't fix.
The big one we watch out for is called Cauda Equina Syndrome. It's rare, but it happens when the nerve roots at the very base of your spinal cord get severely compressed. This is a true medical emergency, and acting fast is critical to prevent permanent damage like paralysis.
If you experience any of the following, don't second-guess it. Go straight to the nearest emergency room.
I know these symptoms sound terrifying, and they are serious. But it's crucial to remember how incredibly uncommon they are. The vast, vast majority of people with a herniated disc will never encounter them.
Let's look at the numbers, because they tell a powerful story. A massive 2020 study analyzed nearly 280,000 people with lumbar disc herniations and found that an incredible 97% recovered fully without surgery. That statistic should give you a lot of confidence in the conservative approach we're discussing. Especially when you consider that back surgery has a 10-40% failure rate, leading to what's known as "failed back surgery syndrome." You can discover more about these recovery statistics to see the data for yourself.
Knowing these red flags isn't meant to undermine the optimism of a non-surgical recovery. Think of it as being fully informed. It empowers you to confidently manage your own healing, while also knowing exactly where the line is—the point where you need to take immediate, different action. This balance of hope and vigilance is what leads to a safe and successful outcome.
Navigating a slipped disc recovery without surgery brings up a lot of practical questions. As you move through the healing process, it's completely normal to wonder about timelines, limitations, and what "normal" progress really feels like. Here are some straightforward answers to the concerns we hear from patients every single day.
Most people start to notice a real drop in that sharp, debilitating pain within the first 6 to 12 weeks of starting a consistent, targeted treatment plan. But it's important to understand this is just the initial relief phase.
Everyone’s timeline is a bit different. It really depends on the severity of the disc injury, your overall health, and just how committed you are to the plan.
Full functional recovery—getting back to all your normal activities without that nagging fear of re-injury—takes longer. You should really be thinking in terms of 3 to 6 months or more to build true, lasting resilience in your spine. Patience here is everything; it’s your best defense against setbacks.
Believe it or not, yes. The body has a remarkable, built-in capacity to heal itself. Over time, it can often reabsorb the bulging disc material in a process called spontaneous regression. But simply waiting and hoping for the best is a gamble.
Guided treatments like spinal decompression, gentle chiropractic adjustments, and specific exercises don't heal the disc for you. Instead, they create the perfect environment for your body to do its job. We're talking about reducing nerve pressure, managing inflammation, and correcting the underlying mechanical issues that led to the problem in the first place.
Absolutely, but with one huge caveat: you have to be doing the right kind of exercise. Just hitting the gym or trying random stretches you saw online can easily make things a whole lot worse. A trained professional is essential here to prescribe gentle, specific movements that stabilize your core muscles without putting any strain on that injured disc.
Safe and beneficial activities almost always include:
These controlled movements are a non-negotiable part of a successful non-surgical recovery. They're what help you build a stronger, more supportive spine for the long haul.
At Bonesetters Critical Chiropractic, we specialize in creating personalized, non-surgical recovery plans that get to the root cause of your pain. If you're ready to find lasting relief and get your life back, you can explore our evidence-based treatments.