A multidisciplinary approach to pain management isn't just about seeing different specialists; it's about a dedicated team of experts working together on your specific case. They build a single, unified plan that tackles chronic pain from every angle—physical, psychological, and even lifestyle-related—to help you find real relief and get your life back.

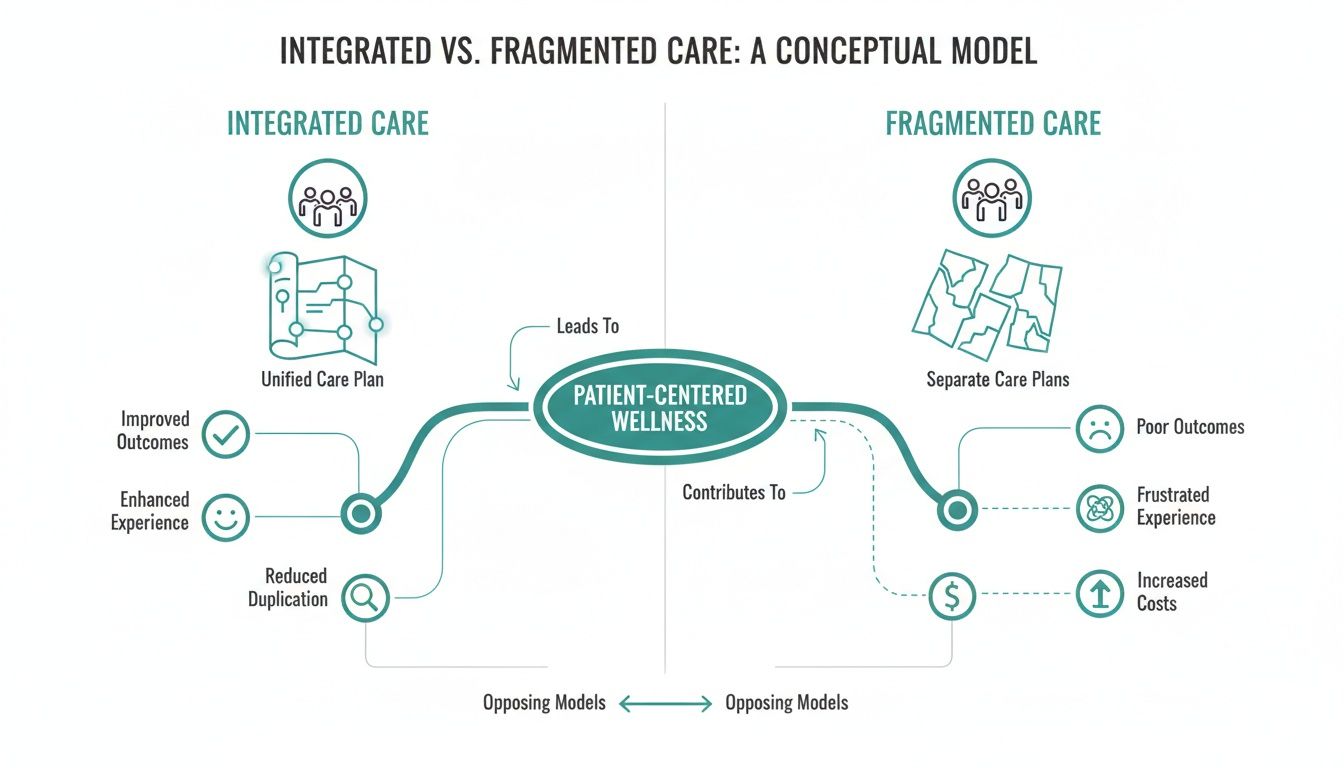
If you're dealing with chronic pain, you probably know the drill. You see one doctor for medication, a physical therapist for exercises, and maybe another specialist for injections. Each appointment can feel like a separate, isolated event. You find yourself retelling your story again and again, with no single person looking at the whole picture.
This scattered approach often falls short because chronic pain is almost never a simple, one-dimensional problem. It’s more like a tangled knot with multiple threads. Pulling on just one thread—like only using medication—might loosen it for a moment, but it won’t undo the knot.
Treatments that stand alone tend to do one thing: mask symptoms. They rarely get to the web of root causes that keep chronic pain going. Think about all the ways pain affects your life.
When a treatment focuses on just one of these areas, the others are left to run wild, and the pain cycle continues. For instance, medication might calm an inflamed nerve, but if the poor posture or spinal misalignment causing that inflammation isn't addressed, the pain will just come right back. You can learn more about how these issues connect in our guide on the best treatment for nerve pain.
A multidisciplinary team acts like a master mechanic for your body, bringing together different specialists who all understand the full machine. Chiropractors, physical therapists, pain medicine doctors, and psychologists communicate and collaborate, working from the same game plan. Your plan.
This coordinated strategy does more than just chase symptoms; it aims to restore function, improve your quality of life, and treat you as a whole person. It’s built on the understanding that true healing happens when the body and mind are on the same page.
Take whiplash, for example. We know that just treating the neck strain often isn't enough. Lasting recovery frequently requires dedicated support for the mental and emotional side of the injury, which is why emotional trauma recovery for whiplash is so critical. A team-based approach makes sure no piece of the puzzle is overlooked.
When we talk about a multidisciplinary approach to pain management, we're not just talking about seeing a few different doctors. It’s about building a single, coordinated team that works from the same playbook—a playbook designed just for you. Think of it as a unified strategy, not just a series of disconnected appointments.
Imagine building a custom house. You want the architect, builder, electrician, and plumber all working from the same set of blueprints. They talk to each other, making sure the wiring is done before the drywall goes up and the pipes align perfectly with the foundation. The result is a solid, functional home built right the first time.
Now, imagine if they all worked in isolation. The electrician drills through a newly installed pipe, and the builder frames a wall right where a window was supposed to go. That's what fragmented healthcare feels like: chaotic, frustrating, and ultimately, ineffective. Treating chronic pain the right way requires that same level of teamwork.
The real power of a multidisciplinary model comes from its core principles. It’s a structured, intentional method for tackling pain from every possible angle. A big part of this is effective care coordination, which is the glue that holds your entire treatment plan together.
This integrated system stands on three pillars:
This philosophy shifts the focus from simply treating a symptom, like a herniated disc, to caring for the person who is living with the effects of that injury.
The need for this kind of coordinated care has never been clearer. Chronic pain affects an estimated 100 million Americans, yet the healthcare system is falling behind. This has created a massive shortage of programs, with only about one specialized interdisciplinary center for every 1,724,137 people in pain. That’s a staggering gap.
This scarcity really drives home the value of clinics that can bring multiple therapies together. For example, combining state-of-the-art diagnostics with treatments that address both structural problems and inflammation often leads to far better outcomes. To see how one specific modality fits in, check out our guide on cold laser therapy for pain relief.
Integrated care isn't about having more specialists; it's about having them work as one unified team for you.
Ultimately, a true multidisciplinary approach creates a smoother, more supportive, and much more effective path to feeling better. It ensures that every step you take is a deliberate move forward, guided by a team that sees the whole you and is fully committed to getting you back on your feet.
A multidisciplinary approach to pain isn't just a buzzword; it's a team of real-life specialists working together, for you. Think of them as a pit crew for your body—each member has a specific job, but they all work in perfect sync to get you back in the race.
Let's move beyond job titles and look at the core function each expert plays in your recovery. When their unique skills and perspectives are combined, the result is far more powerful than any single treatment could ever be on its own. It's this synergy that makes all the difference.
To really understand how this works, it helps to see how each specialist fits into the bigger picture. The table below breaks down the primary focus and common treatments for each member of a coordinated care team.
| Specialist Role | Primary Focus | Common Treatments | How They Collaborate |
|---|---|---|---|
| Chiropractor | Restoring structural alignment, joint motion, and nervous system function. | Spinal adjustments, spinal decompression, soft tissue therapies. | Provides structural diagnostics that guide PT exercise plans and inform the pain physician of mechanical nerve irritation. |
| Physical Therapist | Rebuilding strength, stability, and safe movement patterns. | Therapeutic exercises, manual therapy, functional movement training. | Strengthens muscles to support chiropractic adjustments; helps patients regain function after pain physician interventions. |
| Pain Medicine Physician | Managing the biological drivers of pain, like inflammation and nerve activity. | Nerve blocks, epidural injections, medication management. | Reduces severe pain and inflammation, creating a window for the patient to engage effectively in chiropractic and PT. |
| Psychologist | Addressing the mental and emotional impact of chronic pain. | Cognitive Behavioral Therapy (CBT), mindfulness, stress management. | Provides coping strategies that improve treatment adherence and reduce the brain's perception of pain, supporting all therapies. |
| Dietitian/Nutritionist | Optimizing diet to reduce systemic inflammation and support tissue healing. | Anti-inflammatory diet plans, nutritional counseling, supplement advice. | Works with the whole team to create a healing internal environment, which can enhance the effectiveness of all other treatments. |
Each professional plays a crucial part, ensuring that every angle of your pain is addressed—from the physical mechanics to the biochemical and emotional factors.
The foundation of your body's function is its structure—the spine, joints, and the nervous system they protect. As the team's Structural Specialist, a chiropractor is the expert who makes sure this foundation is solid and aligned correctly. Their main goal is to restore proper motion and take pressure off sensitive nerves.
Think of your spine as a superhighway for communication between your brain and body. Misalignments are like traffic jams, slowing down signals and causing pain, weakness, and dysfunction. The chiropractor's job is to clear those jams.
They provide vital information about your body's structural integrity. This helps the physical therapist design exercises that support proper alignment and shows the pain medicine physician where potential mechanical sources of nerve pain are coming from. Choosing the right one is key; you can learn more about how to choose a chiropractor in our detailed guide.
Once your body's structure is better aligned, it's time to rebuild strength, stability, and safe ways of moving. That's the world of the Movement Expert, or physical therapist (PT). Pain often forces us into guarded, awkward movements that actually weaken key muscles and make the problem worse over time.
A PT’s role is to retrain your body to move correctly and efficiently again. They are essentially the architects of your physical recovery, building you back up one step at a time and ensuring the benefits of your chiropractic care last longer.
A physical therapist does more than just give you exercises; they rebuild your confidence in your body’s ability to move without fear or pain.
By strengthening the muscles around the affected area, a PT creates a strong, stable support system that helps prevent future injuries.
Sometimes, the biological sources of pain—like severe inflammation or nerves that just won't quiet down—require direct medical intervention. The Nerve and Inflammation Expert, a pain medicine physician, specializes in pinpointing and calming these biological fires.
They use advanced diagnostics and highly targeted treatments to bring relief, especially when pain is so intense it stops you in your tracks. Their work can create a crucial window of opportunity, dialing down the pain enough for you to fully participate in your chiropractic and physical therapy sessions. They work closely with the whole team, often targeting a specific compressed nerve a chiropractor has identified to make subsequent treatments more effective.
Chronic pain is never just physical. It takes a huge toll on your mental and emotional health. The Mind-Body Strategist, a psychologist specializing in pain, helps you handle the stress, anxiety, and frustration that almost always come with long-term pain.
This is a critical piece of the puzzle. They give you practical tools to break the vicious cycle where pain fuels stress, and stress then fuels more pain. By helping you reframe your relationship with pain, they empower you to take back control of your life.
As you can see, this kind of integrated care is built around a single, unified plan. It ensures every specialist is pulling in the same direction—toward your recovery. Psychological support isn't an add-on; it's a vital part of a complete, whole-person healing plan.

It’s one thing to talk about theories and principles, but what does a multidisciplinary approach to pain management actually look like for a real person? Let’s walk through the story of James, a 48-year-old architect whose life was derailed by chronic low back pain. An avid hiker, James suddenly found himself sidelined by a nagging disc injury that turned his favorite pastime into a painful memory.
His first attempts at getting help felt like a frustrating maze of disconnected appointments. One doctor prescribed muscle relaxants, while a different therapist handed him a generic sheet of exercises. Nothing was connected, and James felt less like a person and more like a collection of symptoms. Discouraged, he decided to try a clinic that offered a truly integrated model of care.
James’s first appointment was nothing like he’d experienced before. Instead of a quick, siloed exam, he met with a team of specialists at the same time: a chiropractor, a physical therapist, and a pain medicine physician. They didn't just glance at his MRI—they listened to his whole story. They heard about his demanding job, his abandoned hiking trips, and the constant fear of making the pain worse.
This collaborative assessment gave them a 360-degree view of the problem.
Working together in the same room, they built a single, unified plan. It wasn't three separate treatment paths running in parallel; it was one cohesive strategy designed from the ground up to get James back on the trail.
The real magic happened in how the treatments were timed and coordinated. James’s therapies were carefully sequenced to build on one another, creating a healing momentum that isolated appointments could never achieve. His weekly schedule became a clear roadmap to recovery.
For instance, on a Tuesday, he might first see the pain medicine physician for a targeted injection to calm the severe nerve inflammation. This created a crucial window of relief.
Just two days later, with the inflammation down, he’d see his chiropractor for gentle spinal decompression. This treatment was now far more effective at taking pressure off the injured disc. Right after that session, he’d head over to the physical therapist to work on specific core-strengthening exercises, which helped stabilize his spine and lock in the benefits of the decompression.
Progress was no longer measured just by a number on a pain scale. It was measured in functional achievements—real-life victories that gave James his world back.
The first milestone was small, but for James, it was huge: he could sit through a two-hour client meeting without constantly shifting in his chair. A few weeks later, he walked his dog for a full mile with no radiating leg pain. The team celebrated these wins right alongside him, adjusting the plan as his body grew stronger.
After three months of consistent, coordinated care, James laced up his hiking boots again. He started with a short, flat trail, his confidence growing with every step. This journey was about more than just eliminating pain; it was about rebuilding trust in his own body.
Six months after that first team assessment, James stood at a scenic overlook, having just finished a five-mile hike. He wasn’t just managing his pain anymore; he was living his life again. His story is a powerful reminder that a true multidisciplinary approach does more than just treat a condition—it restores the whole person.
It’s one thing to talk about the theory of multidisciplinary pain care, but it’s another to see it in action. At our clinic, we’ve taken this concept a step further. Instead of just coordinating with outside specialists, we've built a powerful, integrated care model right here under one roof. Our advanced therapies and diagnostic tools aren't just a collection of services; they were chosen and designed from day one to work together, creating a seamless and effective path to relief.
Everything we do starts with a comprehensive diagnostic deep dive. We look far beyond the surface-level symptoms to get to the interconnected root causes of your pain. This isn't just about spotting a herniated disc on an MRI. It's about understanding the entire biomechanical chain reaction—the spinal misalignments, the resulting nerve pressure, the muscular imbalances, and even the systemic inflammation—that’s preventing you from healing.
Once we have that complete picture, we build a personalized protocol that layers treatments in a very specific and intentional sequence. That synergy is the real secret sauce. Each therapy is selected not just for what it can do on its own, but for how it amplifies the effectiveness of the others.
Our core tools for this integrated model include:
Think about how this plays out for a condition like sciatica. We might first use the PulStar to correct the underlying spinal misalignment that's putting pressure on the nerve root. Next, spinal decompression gently creates more space around that irritated sciatic nerve. Finally, we apply cold laser therapy to calm the inflammation and speed up the nerve's healing process. Each step paves the way for the next one to be even more successful.
By combining these therapies, we're hitting the problem from multiple angles at once—addressing the structural, neurological, and cellular components of pain. It's a true in-house multidisciplinary strategy designed for faster, more lasting results.
Of course, a truly whole-body approach has to look at the body's internal environment, too. Chronic inflammation is a massive driver of persistent pain, and what you eat can either fan those flames or help put them out. That's why nutritional counseling isn't just an add-on service for us; it's woven directly into every single patient's treatment plan.
We provide practical, real-world guidance on anti-inflammatory eating and targeted supplements that support your body’s natural healing processes from the inside out. This nutritional support helps lower systemic inflammation, gives your body the raw materials it needs for tissue repair, and can make a huge difference in your overall outcome.
This integrated model isn't just our philosophy; it reflects a major shift happening across healthcare. The global pain management market is finally moving away from just masking symptoms and toward non-invasive therapies that fix the root cause. In fact, innovative, non-opioid treatments now account for over 70% of all pain therapeutics in development. By focusing on structural correction, inflammation reduction, and nutritional support, our clinic is squarely at the forefront of this forward-thinking approach. You can get more insights on this market shift and its drivers in this detailed industry report.
Taking a new approach to chronic pain always brings up questions. It's only natural. Understanding the process, what's expected of you, and what the journey looks like are crucial for feeling confident and in control. A multidisciplinary approach to pain management is a big leap from what most people are used to, so let's walk through some of the most common questions we hear.
Think of this as building a solid foundation. The more you understand how all the pieces of your care fit together, the more you can become an active partner in your own recovery, and the better your results will be.
This kind of coordinated, team-based care isn't for a simple, acute injury. It's designed for people facing stubborn, complex pain that hasn't gotten better with one-off treatments. If your pain has become a constant presence in your life, dictating what you can and can't do, that’s a major sign you need a more comprehensive strategy.
You're likely a perfect candidate if any of these sound familiar:
Basically, if your pain is messing with your mood, your work, your sleep, and your ability to just enjoy life, a team-based plan is built for you. It's designed to address the entire web of factors causing your pain, not just the one symptom that screams the loudest.
This is a big one. In a multidisciplinary setting, you're not just a passive patient receiving treatment—you are the single most important member of the team. Your active participation isn't just helpful; it's absolutely essential for success.
Think of the specialists as expert guides and coaches. They know the terrain, but you're the one hiking the trail.
Your role really boils down to a few key responsibilities:
You are the central hub of information. Your feedback—what’s working, what isn't, how you're feeling day-to-day—is the critical data the team uses to adjust and perfect your treatment plan. Open and honest communication is your superpower here.
Your success ultimately hinges on your commitment to the unified plan. That means showing up for your appointments, doing your home exercises diligently, and making the lifestyle and nutritional changes the team recommends. When you take ownership of your role, you become a true partner in your own healing, which is an incredibly empowering feeling.
This might be the most important distinction to grasp. The difference comes down to one word: coordination.
When you see multiple specialists on your own, you often get fragmented care. You're stuck in the middle, trying to relay what the chiropractor said to the physical therapist, who might give you conflicting advice. One doctor says to rest, another says to exercise, and you're left confused, frustrated, and in pain.
A true multidisciplinary approach gets rid of that chaos.
It’s the difference between a pit crew where every member works in perfect sync, and a group of individual mechanics all trying to fix the same car without ever talking to one another.
Insurance coverage can definitely vary depending on your specific plan and provider. The good news is that many of the individual services within an integrated program—like chiropractic care and physical therapy—are often covered benefits under most insurance plans.
That said, it’s always best to get clarity before you start. We strongly recommend calling your insurance provider to understand your specific benefits for each specialist you'll be seeing. Our administrative team is also very skilled at navigating these questions and can help you make sense of your policy to ensure there are no surprises down the road. That way, you can focus on what really matters: getting better.
At Bonesetters, our entire model is built to provide this kind of coordinated, whole-body care all under one roof. We combine advanced diagnostics with a blend of therapies designed to work in synergy, addressing the root cause of your pain instead of just chasing symptoms. If you're ready to move past fragmented treatments and see what a truly integrated approach can do, we invite you to explore our evidence-based protocols.