
If you’re dealing with a meniscus tear, the first question on your mind is probably, "Can I fix this without surgery?" The answer, for many people, is a resounding yes. Treating a meniscus tear without surgery isn't just a possibility; it's often the most effective and sensible path back to a healthy, functional knee. This approach is all about working with your body's natural healing abilities, using proven conservative methods to get you moving again and provide lasting relief.

For a long time, the knee-jerk reaction to a torn meniscus was to schedule a surgery. But our understanding has evolved significantly, and the medical consensus has shifted. Today, a mountain of evidence points to conservative care as the first and best option for a huge number of cases—especially for the degenerative tears that are incredibly common in adults over 35.
This shift comes from a simple but critical realization: cutting out pieces of the meniscus can actually fast-track knee arthritis. Think of the meniscus as your knee's primary shock absorber. When you remove it, you're forcing the bones to grind against each other, which only causes more problems down the road.
Study after study has shown that non-surgical strategies can deliver results that are just as good as—and sometimes even better than—going under the knife. The goal isn't just to "fix" what's on an MRI; it's about true functional recovery. We're talking about rebuilding strength, regaining stability, and achieving pain-free movement.
This isn't just a niche opinion. A major international agreement, the 2024 EU-US Meniscus Rehabilitation Consensus, now formally recommends non-operative treatment as the premier approach for degenerative meniscus tears. The analysis confirmed what many of us have seen in practice for years: physical therapy alone often matches surgery in relieving symptoms and restoring function, all while avoiding the risk of accelerated osteoarthritis. You can read more about these game-changing findings in the 2024 Meniscus Rehabilitation Consensus.
Choosing a non-surgical path isn't about "doing nothing." It's an active, strategic process designed to build a stronger, more resilient knee joint that can support you for years to come without the risks of an operation.
Deciding between surgery and a more conservative route can feel overwhelming. To make it clearer, let's break down the key differences.
| Aspect | Non-Surgical Treatment | Surgical Treatment (Meniscectomy/Repair) |
|---|---|---|
| Primary Goal | Restore function, build strength, manage pain, and promote natural healing. | Physically remove or repair the torn meniscus tissue. |
| Typical Candidate | Most degenerative tears, many smaller acute tears without locking symptoms. | Large, complex tears causing mechanical locking, or cases unresponsive to conservative care. |
| Key Methods | Physical therapy, bracing, activity modification, injections, lifestyle changes. | Arthroscopic meniscectomy (trimming) or meniscus repair (stitching). |
| Recovery Time | Varies, but functional improvement can be seen in weeks. Full recovery may take months. | 4-6 weeks for meniscectomy; 3-6 months or more for a repair. |
| Major Risks | Low risk; primarily related to improper exercise or slow progress. | Infection, blood clots, nerve damage, stiffness, and accelerated arthritis (meniscectomy). |
| Long-Term Outlook | Excellent for preserving joint health and preventing future arthritis. | Mixed. Repair has better long-term outcomes, but meniscectomy is linked to a higher risk of osteoarthritis. |
This table gives you a quick snapshot, but remember that every knee is different. The best path for you depends on your specific tear, your activity level, and your long-term goals.
This guide is designed to be your roadmap. We'll walk through the different pieces of an effective non-surgical treatment plan, showing you how they all fit together to help you heal with confidence and get back to doing what you love.

Before we can talk about healing a meniscus tear, we first have to get familiar with what it actually is. Picture your thighbone (the femur) and your shinbone (the tibia) meeting at the knee. Without something in between, these two massive bones would just grind against each other. It’d be bone on bone.
That’s where the meniscus comes in. Each knee has two of these C-shaped wedges of tough, rubbery cartilage. They act as your knee's primary shock absorbers, cushioning the joint with every step you take. Think of them as custom-fit gaskets that spread out the force and keep the joint stable and moving smoothly. They’re absolutely vital.
A meniscus tear isn't a one-size-fits-all injury. They typically happen in one of two ways, and understanding the difference is the first step toward finding the right path forward.
Acute Tears: This is the one you see in sports highlights. An athlete plants their foot, twists, and goes down. That sudden pivot, an abrupt stop, or a deep squat under load can cause a sharp, immediate tear. While common in athletes, an awkward fall or even just stepping off a curb wrong can cause an acute tear in anyone.
Degenerative Tears: These are far more common, especially for anyone over 35. This isn't about one single dramatic event. Instead, it's the result of cumulative wear and tear over decades. The cartilage slowly loses its resilience, becoming more brittle and thin, and can eventually tear from a simple movement like getting out of a car or squatting to pick something up.
Interestingly, many people walking around with degenerative tears have no idea. They don't remember any specific injury, and research shows that a surprising number of adults have these tears without any symptoms at all. This is a game-changer because it tells us the tear itself isn't always the villain—it's often the inflammation and poor mechanics around the tear that cause the pain.
When it comes to degenerative tears, seeing one on an MRI doesn't automatically mean you need surgery. The real goal should be to calm the inflammation and restore proper knee function. This is precisely why exploring meniscus tear treatment without surgery is often the best first move.
While everyone's experience is a little different, there are a handful of classic signs that point to a meniscus tear. Learning to recognize them is like learning to understand what your body is trying to tell you.
Here are the common red flags:
Where you feel the pain can also be a clue. If it's on the inside of your knee, that often points to a medial meniscus tear. Pain on the outside is more likely a lateral meniscus tear.
Once you can identify these symptoms, you're in a much better position to understand a diagnosis and take an active role in the non-surgical healing strategies that can get you back on your feet.

If there's one non-negotiable part of healing a meniscus tear without surgery, it’s a professionally guided physical therapy (PT) program. Think of your knee as a finely-tuned machine. When a critical component like the meniscus gets damaged, the whole system gets thrown out of whack. Physical therapy is the careful process of recalibrating that system—not just to quiet the pain, but to build a more durable, resilient joint for the long haul.
This isn't just about getting a list of exercises. It’s a phased, intelligent approach that adapts as your body heals. The first priority is always crisis management: getting the pain and swelling down while gently getting your knee to bend and straighten again. Only when that foundation is set can the real work of rebuilding begin.
A good physical therapist is your guide, making sure you push the knee just enough to encourage healing without re-injuring it. It's a delicate balance. Pushing too hard, too soon is one of the biggest mistakes people make, and it can set you back weeks.
The core strategy behind physical therapy is strengthening the muscles that support your knee. Your quadriceps, hamstrings, and glutes act as a "natural brace" for the joint. When they're strong and working together, they absorb shock and distribute forces away from the injured meniscus, effectively taking the load off the damaged spot.
Picture your meniscus as a torn cushion in a chair. You can't just stitch it up easily, but you can build a powerful new support frame around it to take most of the weight. That’s exactly what targeted strengthening does. This goes way beyond standard leg day workouts; it's about zeroing in on the specific muscles that have the biggest impact on knee stability.
Key muscle groups your therapist will target include:
By methodically strengthening this muscular network, you create a stable, supportive environment where your meniscus can heal and function without being constantly irritated.
A personalized physical therapy plan doesn't just treat the tear; it corrects the underlying biomechanical problems that might have caused the injury in the first place. This proactive approach is essential for lasting success.
Strength is only half the battle. Another crucial goal of PT is restoring proprioception. It's a fancy word for a simple concept: your body's awareness of its position in space. After an injury, the nerve signals that tell your brain where your knee is can get muddled, leading to that unnerving feeling of instability or the sensation that your knee might "give out."
Proprioception exercises are all about rebooting that brain-body connection. They often involve challenging your balance, which teaches your muscles to react faster to protect the joint.
Common examples include:
This kind of training builds reflexive stability—your muscles learn to fire automatically to protect your knee without you even thinking about it. Rebuilding that confidence in your knee's stability is what ultimately allows you to get back to your life without fear. It's this one-two punch of a strong muscular brace and sharp proprioception that makes physical therapy the true cornerstone of non-surgical meniscus recovery.
Beyond the essential work of physical therapy, we have some incredible tools that can give your body a serious advantage in the healing game. These aren't just about managing symptoms; they work on a cellular level to create the perfect environment for your meniscus to repair itself. This is where meniscus tear treatment without surgery gets proactive, moving from passive waiting to actively promoting regeneration.
One of the most effective techniques is Knee Decompression Therapy. Picture your knee joint as a tightly squeezed sponge. All that pressure from swelling and inflammation makes it impossible for healing fluids to get inside. Knee decompression gently creates negative pressure within the joint, like a subtle vacuum. This pulls nutrient-rich fluids toward the injured meniscus, helping to wash away inflammatory junk and deliver the building blocks needed for repair.
This process does more than just feel good. By taking pressure off sensitive nerves, it eases pain and, critically, rehydrates the cartilage. For a tissue like the meniscus with poor blood supply, this flood of nutrients is a total game-changer.
Another powerful tool in our non-surgical toolkit is Class IV Laser Therapy. Think of the mitochondria inside your cells as tiny batteries that power everything, especially tissue repair. After an injury, these batteries are running on low, making the healing process slow and sluggish.
Class IV Laser Therapy uses specific wavelengths of light that safely penetrate deep into the knee. This light energy is like plugging your cells into a charger, supercharging the mitochondria to produce more ATP—the body's fuel.
This energy surge creates a cascade of benefits:
To get a better feel for how this technology helps, check out our guide on laser therapy for knee pain. It’s a completely painless way to give your body the direct energy boost it needs to heal from the inside out.
This is where things get really exciting. Regenerative medicine, especially Platelet-Rich Plasma (PRP) injections, taps into your body’s innate ability to heal. We take a small sample of your own blood, use a centrifuge to concentrate the platelets, and then inject this super-concentrated healing solution directly into the tear.
So, what’s so special about platelets? They are the body’s first responders, loaded with hundreds of powerful growth factors. When we inject them into the knee, they act like a general contractor on a construction site, shouting out orders to:
It's an incredibly direct and natural approach. We’re simply concentrating your body's best healers and putting them exactly where they need to be. The results we've seen have been fantastic, even for tears that are often considered "surgical only."
A medical review looking at complex bucket-handle tears found surgery had a 14.8% failure rate, which jumped to a shocking 34.2% on follow-up. But a non-surgical approach can tell a different story. One case study followed a 43-year-old with an MRI-confirmed bucket-handle tear who chose this path. After only three PRP sessions over seven months, he was completely pain-free. A follow-up MRI at the 10-month mark confirmed the meniscus had actually healed.
These therapies—decompression, laser, and PRP—aren't isolated treatments. The real magic happens when they're combined in a personalized plan, giving your knee comprehensive support to heal fully and get you back to your life without surgery.
Real, long-term recovery from a meniscus tear goes way beyond what happens in a physical therapist's office. Your daily habits—how you move, what you eat—are what truly create the right environment for your body to heal. This is a huge piece of the puzzle when it comes to successful meniscus tear treatment without surgery.
The first, and most important, change is activity modification. This isn't about becoming a couch potato. It's about getting smarter with your movements to protect your knee while it’s vulnerable.
I often tell my patients to think of their meniscus like a freshly patched tire. You wouldn't immediately take it off-roading, right? You'd stick to smooth, paved roads until the patch fully cures. The same idea applies to your knee. High-impact activities and twisting motions put a ton of stress on the meniscus, and that can easily undo any healing that has started.
Figuring out what to do—and more importantly, what not to do—is critical. Making a few intelligent substitutions in your fitness routine can keep you moving and sane while giving your knee the break it needs.
Here are some practical adjustments I recommend all the time:
The golden rule here is simple: listen to your body. If you feel a sharp pain, a "catching" sensation, or notice more swelling after an activity, that's your cue to back off. Pain is your body's alarm system, telling you you're pushing too hard, too soon.
Just as important as how you move is what you're putting into your body. With a meniscus tear, inflammation is a major source of your pain and stiffness. Adopting an anti-inflammatory diet can be one of the most powerful tools in your recovery toolkit. It gives your body the raw materials it needs to calm things down and start rebuilding.
Think of your body as a construction site. You can't rebuild a damaged structure with shoddy materials. Nutrient-dense, anti-inflammatory foods are the high-grade building blocks your body needs to repair that torn tissue.
Here’s what to focus on adding to your plate:
By actively incorporating these foods, you're not just waiting to heal—you're participating in the process. You can dive deeper into how diet impacts joint pain with these natural remedies for joint inflammation. When you combine smart activity changes with a targeted nutritional plan, you give yourself a powerful, proactive role in your own recovery.
While we've focused heavily on treating a meniscus tear without surgery—and for good reason, as it's the best path for most people—it's just as important to be realistic. A smart, conservative approach also means knowing when to recognize the signs that surgery might actually be the best option. This isn't about pushing you toward the operating room; it's about giving you the full picture so you can make a truly informed decision for the long-term health of your knee.
Surgery is almost never the first answer, especially for the kind of degenerative tears that pop up as we get older. However, some sharp, sudden injuries can create a physical problem inside the joint that no amount of conservative care can solve. The key is knowing what these red flags look like.
Picture your meniscus as a perfectly smooth, C-shaped shock absorber. Now, imagine a large chunk of it tears and flips over, getting wedged in the joint like a rock in a hinge. This is a classic bucket-handle tear, and it creates a true mechanical block. The knee literally gets locked, making it impossible to straighten all the way. No amount of physical therapy or injections can fix a jam like that.
Here are the big indicators that it's time to get a surgical opinion:
This decision tree gives you a quick visual guide for the day-to-day choices that can help or hinder your non-surgical recovery.
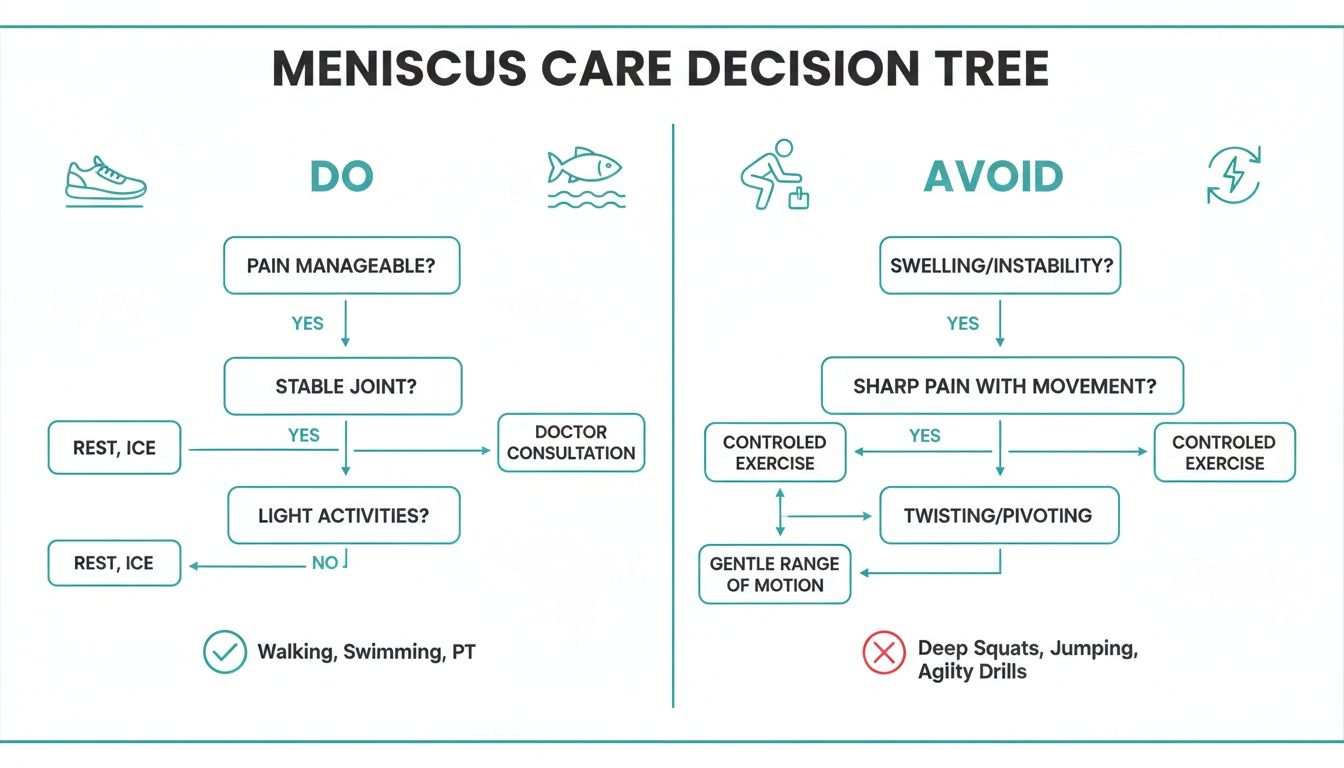
As you can see, the path to healing is paved with low-impact activities and an anti-inflammatory diet, while avoiding the twisting and deep bending that grinds on the injured tissue.
It's critical to understand what "failure of conservative care" really means. It isn't trying a few quad sets for two weeks. It means you've dedicated yourself to a professional, structured program for at least three to six months and have seen almost no change in your ability to walk, climb stairs, or do other daily activities.
Even if you find yourself in this situation, it's vital to explore every possible avenue. Many people fall into a gray area where the injury is serious but not quite an emergency. For those weighing their options, understanding the full spectrum of care is crucial. Learning about powerful alternatives to knee replacement surgery can provide incredibly valuable context and help bridge that gap.
Ultimately, any conversation about surgery should be a collaborative one with your doctor, happening only after you’ve given your body a real, dedicated chance to heal. For the vast majority of people, that committed effort is all it takes to get back to life without ever seeing a scalpel.
It's completely normal to have questions when you're facing a meniscus tear and considering your options. Let's tackle some of the most common ones I hear from patients, so you can feel confident about the path ahead.
There's no single, one-size-fits-all answer here, because every knee—and every tear—is different. Your recovery timeline really depends on a few key things: your age, the specific nature of your tear, and how consistently you stick with your treatment plan.
That said, many people start to feel a real difference—less pain, better movement—within about 4 to 6 weeks of starting a dedicated program. For more significant tears, getting back to most of your normal activities without major issues can take a bit longer, often somewhere in the ballpark of 3 to 6 months of consistent work.
The biggest thing I tell my patients is to be patient with themselves. Healing isn't a race. It's a steady process, and following the plan laid out by your provider is the surest way to get a great result that lasts.
This is a great question, and to answer it, we need to think about "healing" in two different ways: anatomical healing versus functional healing. A large tear that's flipped over and physically locking your knee often needs surgery to fix that mechanical problem.
But for many other tears, the goal of non-surgical care is to achieve functional healing. This means that even if a future MRI shows the tear is still there, you're living a full, active life without pain or instability. By strengthening the muscles around the knee and calming inflammation, we can effectively make the tear irrelevant to your daily function. And that's what really counts.
The goal isn't to get a perfect-looking MRI; it's to get you back to walking, climbing stairs, and enjoying your life without your knee holding you back. Functional recovery is the true measure of success, and it's a realistic goal for the majority of tears.
During the early stages of recovery, protecting your knee is job number one. The main things you want to avoid are movements that put a lot of twisting or grinding pressure on the joint, especially when you're putting weight on it.
Be sure to steer clear of these for a while:
The most important rule? Listen to your body. If you feel a sharp, pinching pain or a "catching" sensation, that's a clear signal to stop. Pain is your body’s way of telling you to back off.
Absolutely. In most situations, gentle walking is one of the best things you can do. Think of it this way: movement is medicine. Walking on a flat, predictable surface gets blood flowing to the knee, which helps bring in the good stuff (nutrients) and clear out the bad stuff (inflammation). It also keeps the joint from getting stiff.
The trick is to do it right. Start with short, easy walks and wear supportive shoes. If you notice more pain or swelling afterward, you’ve likely done a bit too much. Pull back on the distance or check in with your therapist. A few short, comfortable walks throughout the day are far better for healing than one long, painful one.
At Bonesetters, our entire focus is on building personalized, evidence-based plans to help you heal without turning to surgery. If you're looking to explore advanced, non-invasive treatments like Knee Decompression and Class IV Laser Therapy, we're here to help guide you. You can learn more about your path to recovery by visiting us at https://bonesetters.org.