
That sharp, shooting pain, that pins-and-needles sensation, or that frustrating numbness—it's not just a random ache your body came up with. It's a very specific signal. When a nerve gets "pinched," the only way to get lasting relief is to do two things: take the pressure off the nerve and calm the inflammation that pressure has caused.
Often, you can start tackling this right at home with some simple, smart changes like getting proper rest, fixing your posture, and doing a few gentle stretches.

Think about what happens when you put a heavy kink in a garden hose. The water slows to a trickle or stops completely. That's a great way to visualize what’s happening with a pinched nerve. Your nervous system is your body’s electrical wiring, and when a nerve gets squeezed by a bone, muscle, or herniated disc, its signal gets scrambled.
This interference is what causes all those strange and painful sensations.
This pressure doesn't just happen randomly. It's usually the result of something specific, like repetitive work, a sudden injury, or a slow-developing issue like arthritis. Whatever the cause, the pressure messes with the nerve's ability to send clear signals, leading to symptoms that can be anything from a minor annoyance to totally debilitating pain.
You can technically pinch a nerve anywhere, but I see it most often in a few key areas where the anatomy just makes it more likely. Each spot tends to have its own tell-tale signs.
The Big Picture: A "pinched nerve" isn't the final diagnosis; it's a description of the problem. The symptoms—whether it's burning, weakness, or sharp pain—are all direct results of a nerve being physically compressed and unable to do its job.
Once you grasp that, finding a solution becomes much clearer. The pain isn't a mystery; it’s a mechanical problem with a specific cause. The great news is that this means there are specific, highly effective solutions that don’t require surgery. By getting to the root of what’s causing the compression, we can use non-surgical treatments to take the pressure off, let the nerve heal, and get you long-term relief. You're in the right place to find out how.
When that sharp, shooting pain of a pinched nerve hits, what you do in those first few hours can make a world of difference in how quickly you recover. The immediate goals are simple: get the pressure off the nerve and calm down the inflammation. The good news is you can start this process right at home, giving you back a sense of control.
The key concept here is what I call "active rest." This isn't about being completely sedentary for days on end—that can actually make things worse by causing stiffness and weakening the muscles that support the area. Instead, it’s about strategically modifying your activities. You stop doing what hurts, but you keep moving in gentle, restorative ways.
Think of it like this: if sitting at your desk is triggering sciatic pain, maybe you try a standing desk for a few hours or set a timer to get up and walk around every 20 minutes. If turning your head a certain way sends a jolt down your arm, you consciously avoid that motion and make sure you're using a supportive pillow when you rest. It's about being smart, not stationary.
One of the most effective tools in your arsenal is temperature therapy. Using cold and heat correctly, especially in the first 48 hours, can be a game-changer for managing both pain and swelling.
Go Cold First: During that initial flare-up, grab a gel ice pack. Make sure to wrap it in a thin towel (never apply it directly to the skin!) and place it on the sorest spot for 15-20 minutes at a time. The cold constricts blood vessels, which is fantastic for reducing inflammation and swelling. It also provides a welcome numbing effect for some immediate relief.
Bring in the Heat Later: After the first 48 hours, or once that initial, intense inflammation has started to calm down, you can introduce gentle warmth. A heating pad on a low setting for 15-20 minutes will help relax those tight, spasming muscles that are often clamping down on the nerve. The warmth also boosts blood flow, bringing fresh oxygen and nutrients to the area to kickstart the healing process.
There's a right way and a wrong way to do this. For a deeper dive, check out this guide on how to use gel ice packs correctly to get the most out of them.
While you should absolutely avoid any intense exercise, gentle, targeted movements are your friend. The whole idea is to create a little more space around that compressed nerve. You’d be surprised how much relief you can get from simple posture adjustments.
If your low back is the problem, try this: lie on your back with your knees bent and your feet flat on the floor. This simple position can immediately take a significant amount of pressure off your lumbar spine.
Expert Takeaway: Dealing with a pinched nerve often starts with a simple first step: rest. Halting the activities that worsen nerve compression is a top recommendation that allows the nerve to begin its natural recovery. However, proactive care is essential.
Here’s why just waiting it out isn't always the best plan. Studies show that without any real intervention, about 23% of people with nerve compression actually get worse over a two-year period. On the other hand, 48% improve and 29% stay the same. This is why pairing rest with focused care is so critical. At Bonesetters Critical Chiropractic, Dr. Leonard Hayes combines this active rest approach with physical therapy and other advanced therapies, and we see an 83% immediate pain reduction for nerve entrapments—a huge leap over what rest alone can accomplish. You can read more on the findings from the Mayo Clinic about pinched nerve treatment.
You can also start incorporating some very gentle stretches designed to decompress the affected area. The number one rule is to listen to your body—if a movement causes sharp pain, stop immediately.
For Neck Pain (Neck Tilt):
While sitting, gently tilt your head, aiming your left ear toward your left shoulder. You should feel a light stretch, not a sharp pain. Hold for 20-30 seconds, then slowly return to the center and repeat on the right side.
For Sciatica (Knee-to-Chest):
Lie on your back. Gently bring one knee up toward your chest, using your hands to pull it in for a comfortable stretch in your lower back and hip. Hold for 20-30 seconds and then switch legs.
For Carpal Tunnel Symptoms (Wrist Extensor Stretch):
Hold one arm straight out in front of you, with your palm facing down. Use your other hand to gently bend your wrist downward until you feel a stretch in your forearm. Hold for about 20 seconds.
These at-home steps are your first line of defense. They put you in the driver's seat, allowing you to manage your symptoms and create the right environment for your body to start healing.
While tackling nerve pain at home is a great first step, it's just as important to recognize when you're out of your depth. A pinched nerve isn't always something you should handle alone, and knowing the difference between manageable discomfort and a genuine red flag is key to a safe recovery.
Think of it this way: some symptoms are a quiet suggestion to take it easy, while others are a screaming alarm that you need to call a professional. You need to learn how to hear the difference.
Let's get straight to the point. Certain symptoms are non-negotiable and demand immediate medical attention. These are signs of severe nerve compression that could lead to permanent damage if you "wait and see."
Don't hesitate if you experience any of the following:
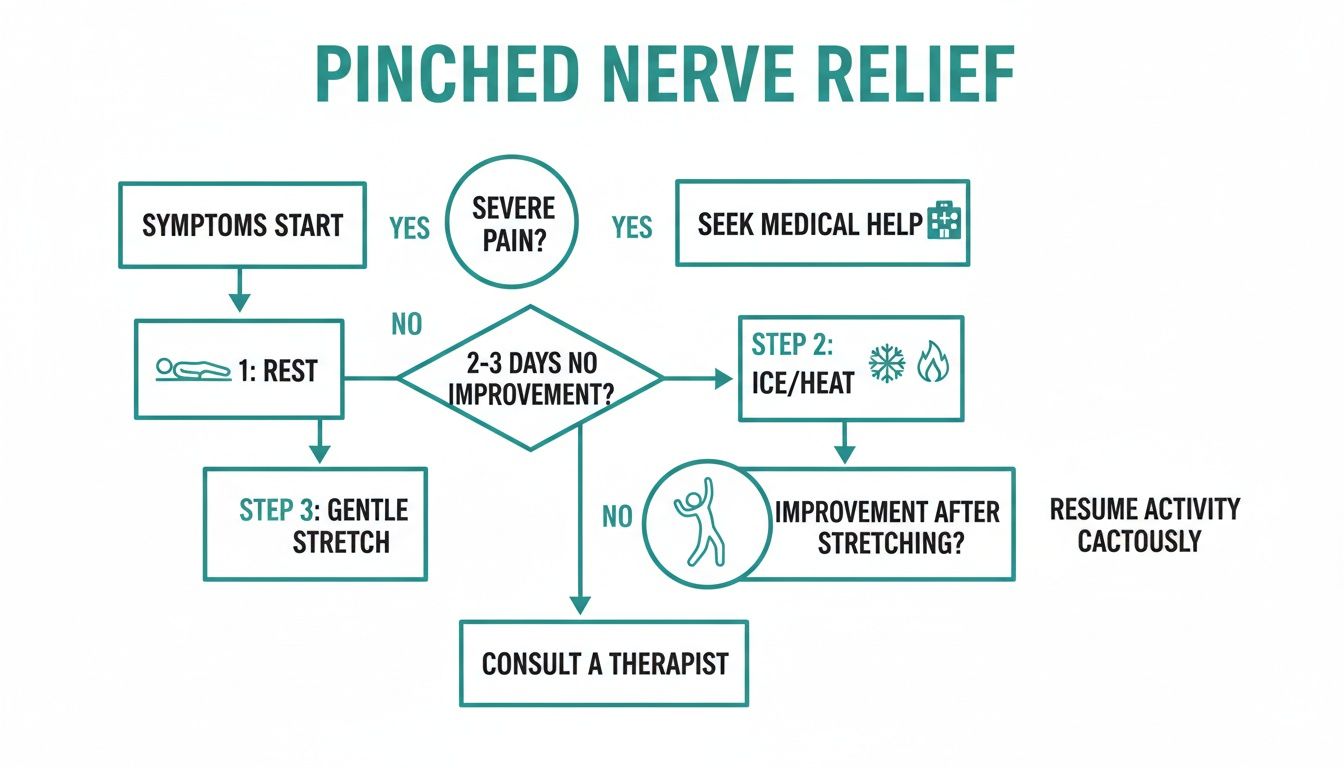
This flowchart lays out the typical path, from initial home care to knowing when it's time to escalate to professional help.
The takeaway here is to start with conservative care, but be ready to pivot and seek help when your body tells you it's time.
To make it even clearer, here’s a quick guide to help you decide on the right course of action based on what you're feeling.
| Symptom | Manage at Home If... | See a Professional If... | Seek Urgent Care If... |
|---|---|---|---|
| Pain | Mild to moderate, improves with rest and ice/heat. | Pain is constant, severe, or lasts more than a week with no improvement. | Pain is sudden, excruciating, or follows a significant trauma. |
| Numbness/Tingling | Intermittent and doesn't affect function. | The sensation is persistent or spreading. | Numbness appears suddenly in the "saddle" region (groin, buttocks). |
| Weakness | You feel a slight lack of power but can still perform tasks. | It's noticeably harder to lift things or perform daily activities. | There is a sudden and significant loss of strength (e.g., foot drop). |
| Function | You can still work and perform daily routines with some discomfort. | The pain is interfering with sleep, work, or hobbies. | You experience a sudden loss of bladder or bowel control. |
This table isn't a substitute for a diagnosis, but it's a solid framework for making smart decisions about your health.
Beyond the red flags, there are other clear signs that home remedies have hit their limit. You've given it a fair shot, but the problem isn't going away.
I see it all the time in my practice: people wait until the pain is unbearable before seeking help. Proactive care is always a better strategy. If your symptoms are consistently disrupting your life—ruining your sleep, making work a misery, or keeping you from your favorite activities—it's time for an expert opinion.
Book a consultation if you find that:
When symptoms linger or recur, it usually points to an underlying mechanical issue that simple rest and stretching can't fix. A specialist can get to the root of the problem—whether it's a disc herniation, spinal stenosis, or something else entirely. Finding the right person is crucial, so it’s worth learning how to choose a chiropractor who can give you an accurate diagnosis and a targeted plan to finally resolve the issue.

So, you've tried the ice packs, the stretches, and the activity modifications, but that nagging pain from your pinched nerve just won't quit. When at-home care only offers temporary relief, it’s a strong signal that the underlying mechanical problem needs a more direct, powerful solution.
This is where advanced non-surgical treatments come in. These aren't about just masking pain; they are highly targeted therapies designed to get to the root cause of the nerve compression. The goal is to correct the problem—be it a bulging disc, inflammation, or a stuck joint—and allow your body to truly heal for good, all without invasive procedures.
Let’s dive into some of the most effective, modern options available for anyone wondering how to treat a pinched nerve when the basics just aren't cutting it.
That sharp, shooting pain down your leg from a pinched nerve in the low back is incredibly common. In fact, global health data suggests as many as 619 million people have dealt with back pain tied to nerve issues, often caused by bulging discs putting pressure where it doesn't belong.
Non-surgical spinal decompression has become a go-to for this, boasting an impressive 80% success rate in relieving this kind of pain. Best of all, most people can get right back to their day after a session. This therapy is a true game-changer for conditions like sciatica or radiculopathy.
Here’s how it works: you lie on a specialized table that gently and precisely distracts, or stretches, the spine. This creates a vacuum effect inside the targeted disc.
Key Takeaway: Picture a dried-out sponge. When you submerge it in water, it plumps back up. Decompression does something similar for your spinal discs. The negative pressure helps pull water, oxygen, and nutrients back in, promoting healing and helping the bulging material retract away from the nerve.
This whole process is computer-controlled, ensuring the pull is perfectly tailored to your body and condition. Most people find it quite relaxing—like a gentle, focused stretch.
While traditional chiropractic adjustments are a powerful tool, technology has given us ways to be even more precise and gentle. The PulStar is an FDA-backed system that uses a handheld instrument to analyze and treat restricted joints, not just in the spine but in the extremities, too.
Instead of a manual "popping" or "cracking," the PulStar delivers a series of soft, computer-guided impulses to the stuck joint.
This method is incredibly targeted, focusing only on the joints that need help. Because it’s so gentle, it’s a fantastic option for anyone who might be nervous about traditional adjustments or is currently in a lot of pain. Restoring normal joint function is key to taking mechanical stress off the nearby nerves.
Inflammation is a huge part of the pain equation with a pinched nerve. Class IV Cold Laser Therapy is one of the best tools we have for tackling that inflammation right at the source. It’s a non-invasive treatment that uses specific wavelengths of light energy to penetrate deep into the tissue surrounding the compressed nerve.
This light energy gets absorbed by your cells and triggers a process called photobiomodulation. In simple terms, it gives a massive energy boost to your cells' mitochondria—their little powerhouses.
This cellular jump-start delivers a few key benefits:
The treatment itself is painless. At most, you might feel a gentle warming sensation. If you’re curious about the science, you can read more about how cold laser therapy works to promote healing and ease pain on a cellular level.
Sometimes, an irritated nerve gets stuck in a feedback loop, sending out constant, frantic pain signals. Horizontal Stimulation therapy is specifically designed to break that cycle. It uses unique electrical frequencies that are more compatible with the body than older forms of e-stim, helping to interrupt those pain signals and calm the overactive nerve.
Finally, we can't forget that healing is an inside job. Nutritional support plays a vital role in reducing body-wide inflammation and giving your tissues the raw materials they need for repair. A specialist might recommend specific anti-inflammatory supplements or dietary tweaks to create an internal environment that supports and speeds up your recovery from a pinched nerve.
Getting over a pinched nerve is more than just making the pain go away. It’s about following a smart, structured path that fixes what went wrong in the first place and keeps it from happening again.
It helps to think of recovery in a few distinct stages. Knowing what to expect helps you set realistic goals and see the progress you're making, even when it feels slow. This isn't something that just happens to you; it's a partnership. Your commitment to the plan is every bit as important as the treatments we provide.
Right out of the gate, our only goal is to get you some relief. We need to calm down the inflammation and reduce your pain, and this initial phase can last anywhere from a few days to a couple of weeks.
Think of it like firefighting. We aren't rebuilding the house yet; we're just focused on extinguishing the flames so the real work can begin. Treatments here are gentle and aimed at taking pressure off that irritated nerve. This is often where you’ll feel the most dramatic shift as that sharp, debilitating pain finally starts to back off.
Your job here is pretty straightforward but incredibly important:
Once the initial crisis is over and your pain is more manageable, we pivot. Now, the focus is on fixing the mechanical issue that caused the pinched nerve to begin with. This is the longest and most critical part of your recovery, often taking several weeks.
Whether it’s a misaligned joint, a bulging disc, or a chronic muscle imbalance, this is where we work on lasting structural change. Therapies like non-surgical spinal decompression, computer-guided adjustments, and Class IV cold laser therapy are the heavy lifters during this stage. They’re designed to do more than just mask symptoms.
Progress here isn't just about your pain score going down. We're looking for tangible improvements in your function:
Your Role in Healing: Consistency is the name of the game here. Each treatment builds on the one before it, so keeping your appointments is crucial. This is also when we’ll start introducing specific exercises to support the work we’re doing in the office.
Getting out of pain is fantastic, but staying that way is the ultimate goal. The final phase is all about making sure this problem doesn't come back to haunt you. Once the underlying issue is corrected, we shift to strengthening the muscles that support the area and building up your body's resilience.
The exercises become a bit more challenging, targeting the deep core muscles that stabilize your spine or the specific tissues around the affected joint. We’ll also dive into practical things like ergonomics and posture, making sure your daily habits are helping, not hurting, your recovery.
Success in this phase means you can get back to your life without constantly worrying about a flare-up. It's about being able to take a long walk, sit through a movie, or enjoy your favorite hobby without discomfort. The goal is to make these healthier movement patterns so automatic that they become your new normal.

Getting rid of the pain from a pinched nerve is a huge relief. But the real goal? Making sure it never comes back. The good news is that prevention isn't about some massive, intimidating lifestyle change. It's all about weaving small, smart habits into your day that support your spine over the long haul.
This is where you shift from reacting to pain to proactively taking care of your body. The very same things that helped you heal—creating space for the nerve, easing pressure, and supporting your body's structure—are exactly what you need to do to stay pain-free. It all starts with paying a little more attention to how you move and the environment you're in.
For so many of us, our workspace is ground zero for the repetitive strain that eventually leads to a compressed nerve. A few simple tweaks to your setup can make a world of difference for your neck, back, and even your wrists.
I always tell my patients to set a timer for 30 minutes. When it goes off, just get up and move around for 60 seconds. It's a tiny habit that breaks up static posture, gets your blood flowing, and gives your joints a much-needed reset.
Think of a strong core as your body's natural back brace. It provides incredible stability, taking a huge amount of pressure off your spinal discs and nerves. In the same way, maintaining a healthy weight reduces the constant mechanical stress on your entire frame, from your spine right down to your knees.
You don't need to become a gym rat to see results. Simple exercises can make a profound impact. Things like planks, bird-dog poses, and bridges are fantastic for building that foundational core strength without straining your back.
These aren't just exercises; they're an investment in your body's structural health. When you combine consistent, gentle strengthening with mindful ergonomics, you build a powerful defense. By making these small habits part of your routine, you’re not just crossing your fingers and hoping the pain stays away—you're actively building a more resilient body that can stay comfortable and strong for years to come.
When you're dealing with the pain of a pinched nerve, it's natural to have questions about the recovery process. Knowing what to expect can make a world of difference. Let's tackle some of the most common questions I hear from patients every day.
This is the big one, and the honest answer is: it depends. The severity of the compression and where it's located play a huge role. That said, with targeted non-surgical treatments like spinal decompression and Class IV laser, most people feel a significant drop in their pain within just the first couple of weeks.
But feeling better isn't the same as being fully healed. A complete corrective plan usually takes about 4-6 weeks. This timeline gives us the chance to not only relieve the pressure but to fix the underlying mechanical issue, allow the nerve to fully recover, and strengthen the area so this doesn't happen again.
Absolutely not. The last thing we want to do is cause more pain when you're already suffering. Modern, evidence-based care for a sensitive condition like a pinched nerve is specifically designed to be gentle and comfortable.
At Bonesetters Critical Chiropractic, we've moved past the old ways. We use advanced, computer-guided tools like PulStar for adjustments that are incredibly precise, without any of the forceful twisting, popping, or cracking that people often dread. Patients frequently tell us that treatments like spinal decompression just feel like a gentle, relaxing stretch.
Yes, you can and you should—but you have to be smart about it. This isn't the time to push through the pain. High-impact activities that jar or compress the spine are off-limits for now. Think running, heavy deadlifts, or intense plyometrics. Ignoring this will only set you back.
Gentle movement, on the other hand, is one of the best things for recovery. The right kind of activity gets blood flowing to the nerve, eases stiffness, and builds up the small stabilizing muscles that protect the area. Your doctor will give you a specific list of therapeutic exercises tailored to your situation, but generally, these are great options:
At Bonesetters Critical Chiropractic, we believe in providing clear answers and creating personalized, non-surgical plans that get to the root of your pain. To see how our evidence-based approach can help you, visit us at https://bonesetters.org.