Lasting relief from chronic back pain isn't about just chasing symptoms with temporary fixes. It's about getting to the root of the problem. The most successful approaches I've seen in my years of practice always combine gentle, corrective movement with smart adjustments to your daily life and even some mind-body work to change how you perceive pain.
This isn't a quick fix; it's about building real, long-term resilience.
Before we can even start talking about solutions, we need a clear picture of what we're dealing with. Chronic back pain—the kind that hangs around for more than 12 weeks—is a completely different beast than the acute pain you get from, say, helping a friend move a couch. That acute stuff usually gets better with a few days of taking it easy. Chronic pain, on the other hand, often has deeper, more stubborn causes.
If you're dealing with this, you're in a lot of company. It's a massive global health problem, impacting an estimated 619 million people worldwide back in 2020. It's also the single leading cause of disability. Experts even predict that number could swell to 843 million by 2050 as the global population gets older. You can dig into more of these back pain statistics to see the full scope of the issue.
Getting a handle on where the pain is coming from is our first big step. Most back pain tends to fall into one of two main buckets:
To really get ahead of this, you have to start playing detective. Stop just putting up with the pain and start paying attention to its patterns. For the next week, try keeping a simple log. You don't need anything fancy, just a notebook or a note on your phone.
Jot down the answers to these questions:
This simple act of observation is powerful. It moves you from feeling like a victim of your pain to being an active player in your own recovery. The clues you uncover are gold—they'll help you build a smarter plan and have much more productive conversations with your doctor or therapist.
Expert Insight: Lasting relief from chronic back pain is never about one magic pill or a single treatment. It’s about understanding your personal triggers, figuring out if the cause is mechanical or nerve-related, and then consistently applying the right strategies for you.
When you start to see these patterns, you can finally connect the dots between your daily habits and your pain levels. That's your roadmap for what needs to change.
If you’re living with chronic back pain, you’ve probably been told to "just rest it." But for long-term pain, that's one of the biggest myths out there. While rest is absolutely vital for a fresh, acute injury, extended inactivity can actually make chronic pain worse. The real key is gentle, intentional movement.
This isn’t about gritting your teeth through a hardcore workout. It's about starting slow, building a foundation of stability, and teaching your body it’s safe to move again. Think of it as re-engaging the deep core muscles that act as a natural corset for your spine. When these muscles are weak or switched off—often from years of sitting or an old injury—the big muscles in your back have to pick up the slack, leading to constant strain and pain.
This simple, three-step process is a great way to frame your thinking before you jump into any new exercises. It’s all about listening, identifying what makes things worse, and then getting a professional opinion.
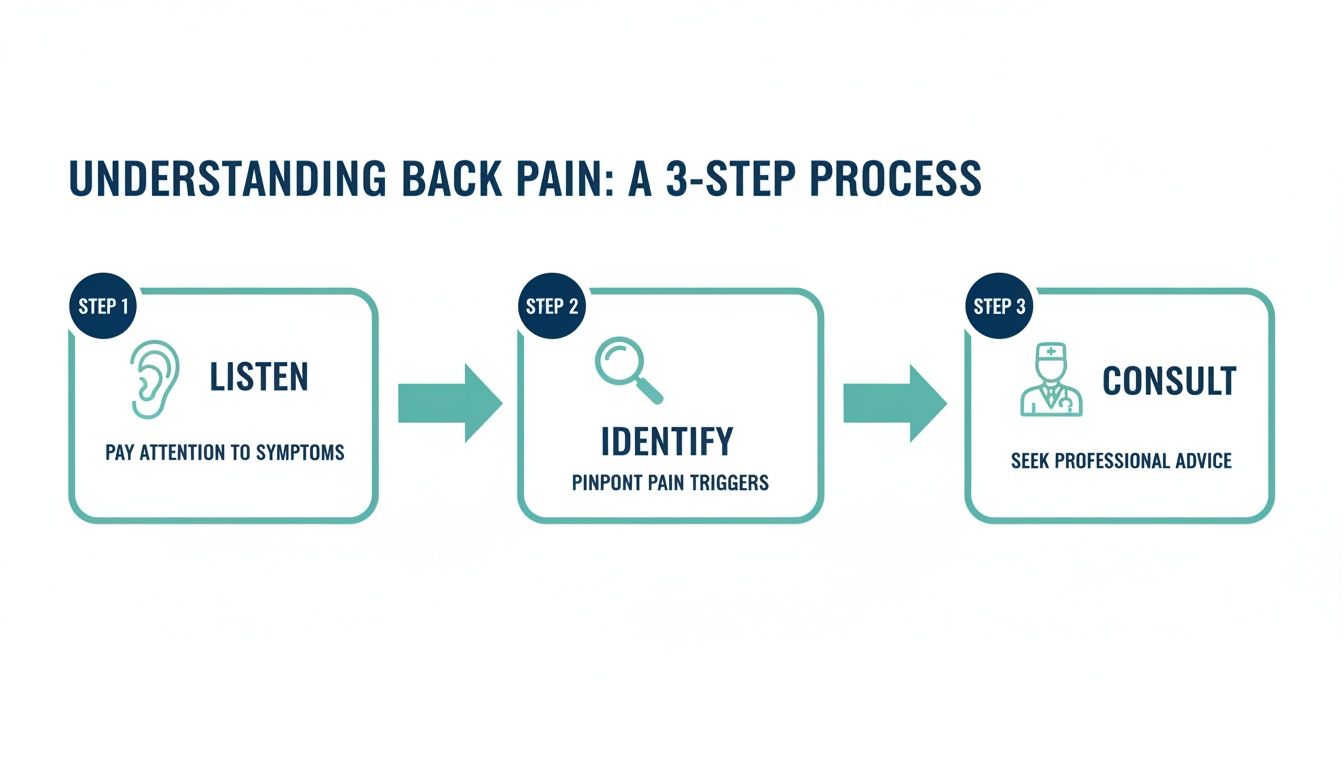
This mindful approach—moving from observation to professionally guided action—is what sets you up for a successful recovery.
The mantra here is consistency over intensity. Seriously, doing a few gentle movements every single day will do more for you than one monster workout a week that leaves you sore for days. These exercises are specifically chosen to wake up your core and encourage spinal mobility without putting any stress on angry, sensitive tissues.
Here are three low-impact movements I always recommend to start with:
A Quick Word on Pain: This is non-negotiable. Your guiding principle should be to listen to what your body is telling you. You should never feel sharp, shooting, or worsening pain during these exercises. A feeling of muscle engagement or a mild stretch is fine, but anything more is your body’s signal to stop or modify.
Lasting change comes from integrating these small movements into your daily life. You don’t need to block out a full hour at the gym. In fact, just 5-10 minutes a day can make a world of difference over time.
Here’s what a simple, effective routine could look like:
This entire approach is backed by what we know works. Global health organizations consistently point to rehabilitation and exercise therapy as cornerstone strategies for pain management. The World Health Organization (WHO) recommends structured rehabilitation plans for all stages of back pain, emphasizing exercises that build strength and flexibility. As you can see in extensive research published on platforms like PubMed, the goal is always to improve function and reduce disability.
Remember, you're not trying to fix everything overnight. The initial goal is to gradually build your body's resilience. By creating a foundation of safe, consistent movement, you start to regain control and prove to yourself that your back can be strong and reliable again.

All the stretching and exercise in the world won't make a lasting difference if your daily environment is constantly working against you. Think about it: your office, your car, even your bed can either be allies or antagonists in your fight against chronic back pain.
The good news is that you don't need a drastic, expensive overhaul. By making small, strategic adjustments to your surroundings, you can dramatically reduce the cumulative strain on your spine and give your body a chance to truly heal.
For so many of us, the desk is ground zero for back pain. Hours spent hunched over a keyboard or craning our necks to see a monitor creates a constant, low-grade strain that feeds the chronic pain cycle. A few simple ergonomic tweaks can change everything.
Start with your chair. Your feet should be flat on the floor with your knees at a comfortable 90-degree angle. If your feet are dangling, grab a footrest. Your lower back needs support, too; if your chair doesn't have it built-in, a small rolled-up towel or a dedicated lumbar pillow works wonders.
Now, look at your screen. The top of your monitor should be at or just below eye level. This simple change stops you from looking down all day. Your keyboard and mouse should be close enough that your elbows stay relaxed by your sides, not reaching forward.
Key Takeaway: The whole point of an ergonomic setup is to bring your work to you, not force your body to contort to reach your work. Your spine should feel neutral and relaxed, not tense.
Creating a truly ergonomic workspace can feel overwhelming at first. This checklist breaks it down into simple, actionable steps. Use it as a quick reference to audit your current setup.
| Setup Element | Optimal Position | Common Mistake to Avoid |
|---|---|---|
| Chair Height | Feet flat on the floor, knees at a 90-degree angle. | Sitting too high with feet dangling or too low with knees above hips. |
| Lumbar Support | A gentle curve supports your lower back's natural arch. | Slouching in a chair with no support, creating a "C" shape in your spine. |
| Monitor Position | Top of the screen is at or just below eye level. | Monitor is too low, forcing your neck to crane downward constantly. |
| Keyboard & Mouse | Close enough to keep elbows bent at 90 degrees, close to your body. | Reaching far forward for the keyboard, causing shoulder and upper back strain. |
| Armrests | Shoulders are relaxed; arms are gently supported. | Armrests are too high (shrugging shoulders) or too low (slumping). |
Reviewing this list once a week can help you catch bad habits before they set in and undo your progress.
Ergonomics isn't just for the office. The way you handle everyday tasks—from driving to doing chores—plays a massive role in your back health. These little moments add up, so learning to move mindfully is a crucial piece of the puzzle.
Think about these common scenarios:
You spend about a third of your life in bed, making your sleep setup one of the most powerful tools for recovery. The right position allows your muscles to relax and your spinal discs to rehydrate overnight. The wrong one can leave you feeling stiff and sore before your day even begins.
If you're a back sleeper, a pillow under your knees is a game-changer; it helps maintain the natural curve of your lower back. For side sleepers, a pillow between your knees keeps your hips, pelvis, and spine in better alignment. If you can, try to avoid sleeping on your stomach, as it puts the most strain on your neck and back.
Finding the right mattress and pillow is also key. Your mattress should be firm enough for support but have enough give to contour to your body. Your pillow should support the natural curve of your neck, not prop your head up at an awkward angle.
While heat can be a fantastic way to soothe chronic muscle tightness, an acute flare-up or fresh injury often needs the opposite approach. Knowing how to use cold therapy is an invaluable skill. You can find a great breakdown on using gel ice packs as an at-home healing modality to calm inflammation effectively. By mastering both your daily environment and your at-home care, you build a powerful, supportive system for lasting relief.

Chronic back pain is never just a physical problem. It’s an experience that weaves itself into your mind and emotions, creating a frustrating cycle where stress and anxiety make the physical sensations feel even worse. This is where we can step in and use the powerful mind-body connection to regain a sense of control.
Think of your nervous system as a highly sensitive alarm. When you’re constantly stressed or anxious, that alarm is dialed way up, making you more sensitive to every pain signal. Mind-body techniques are all about learning how to turn down the volume on that alarm, calming the nervous system and fundamentally changing your relationship with pain.
Stress is a huge amplifier for chronic pain. When you're stressed, your body pumps out hormones like cortisol, which increases inflammation and tightens muscles—directly fueling your back pain. Getting a handle on your stress response is a critical piece of the puzzle.
One of the most immediate tools you have is simple, deep breathing. When you consciously slow down your breath, you tap into the parasympathetic nervous system, your body's built-in "rest and digest" mode. This sends a powerful signal to your brain that you're safe, which can help ease muscle tension and dial down the intensity of pain signals.
Mindfulness meditation is another game-changer. This isn't about clearing your mind of all thoughts. It’s about learning to observe your thoughts and physical sensations without judging them. Research actually shows that a regular mindfulness practice can change the structure and activity in the parts of your brain that process pain.
Expert Insight: The point of mindfulness isn't to force the pain to disappear. It's about creating some mental breathing room between you and the sensation. This allows you to respond with calm awareness instead of with that automatic reaction of tensing up and spiraling into distress.
Sleep is when your body does its most important repair work. But for anyone dealing with chronic back pain, getting that restorative sleep can feel impossible. Pain keeps you up, and a bad night's sleep makes you more sensitive to pain the next day. It’s a vicious cycle.
Improving your sleep hygiene is absolutely non-negotiable for recovery. This just means creating a consistent, relaxing routine that tells your body it’s time to power down.
Here are a few practical tips to get started:
What you eat has a direct line to your body's inflammation levels, and chronic inflammation is a key driver behind many types of back pain. A diet loaded with sugar, processed junk, and unhealthy fats can keep your body in a constant state of low-grade inflammatory stress.
On the flip side, an anti-inflammatory diet can be a powerful way to calm your system from the inside out. This doesn’t mean you have to go on some radical, restrictive diet. It’s about making smart, consistent choices to bring more healing foods into your daily routine.
Think about adding more of these anti-inflammatory powerhouses to your meals:
By weaving these mind-body strategies together—managing stress, prioritizing sleep, and eating to reduce inflammation—you create a powerful internal environment that supports healing and gives you more control over your chronic back pain.
So, you’ve been diligent. You've been doing the gentle exercises, you’ve dialed in your ergonomics at your desk, and you've even started exploring mind-body strategies. But the pain is still there. If that sounds familiar, don't get discouraged. This isn't a sign that you've failed; it's a clear signal that it’s probably time to look into professional treatments that can get to the deeper, more stubborn source of the problem.
Taking that next step can feel big, but it’s a positive move. It means having real conversations with specialists who can give you a more precise diagnosis and introduce you to a whole new range of solutions. The ultimate goal here isn't just to put a temporary band-aid on the pain, but to find a treatment that works with your body’s own healing ability to create lasting change.
For most people, the journey starts with their primary care doctor. They're your first line of defense, helping to rule out any serious underlying conditions and often referring you to a specialist like a physical therapist, rheumatologist, or orthopedic surgeon. The focus, almost always, begins with conservative, non-invasive methods first.
And for good reason. These strategies have a real, measurable impact. For instance, well-designed exercise therapy has been shown to deliver around a 30% improvement in both pain scores and functional ability for people with chronic low back pain. Research from organizations like the International Association for the Study of Pain continues to highlight how these approaches make a global impact on reducing disability.
But what happens when that's not enough? Your doctor might start to discuss other options.
A Key Insight: It's helpful to think of injections and medications as tools to "break the pain cycle." By knocking the pain down a few notches, they create a window of opportunity for you to engage more effectively in the therapies that create long-term change, like physical therapy and targeted exercise.
For many people dealing with nagging conditions like a herniated disc, spinal stenosis, or sciatica, the conversation eventually turns to surgery. Before you go down that road, you should know there’s a growing world of advanced, non-surgical treatments out there. These are designed to fix the root mechanical problems without the risks and lengthy recovery of an invasive procedure.
These modern therapies are all about creating the perfect environment for your body to heal itself. They aren't just masking symptoms; they're aimed at correcting the underlying dysfunction.
If you're dealing with disc pain, this is a game-changer. Spinal decompression therapy uses a highly specialized, computer-guided table to apply a gentle, precise pulling force to the spine.
This process carefully coaxes the vertebrae apart, which creates negative pressure inside the disc—think of it like a subtle vacuum effect. This can help pull bulging or herniated disc material back where it belongs while also drawing in oxygen and nutrients essential for healing. The whole process is slow, controlled, and actually quite comfortable. To see exactly how this works, you can review our comprehensive disc care protocol that breaks down the entire approach.
You might have heard this called "cold laser" therapy. This treatment uses very specific wavelengths of light that penetrate deep into injured tissue. Unlike a surgical laser, it doesn't cut or burn. Instead, it sparks activity at the cellular level.
This light energy gets to work in a few key ways:
These therapies, along with others like computer-guided adjustments and horizontal stimulation, represent a huge leap forward in our ability to relieve chronic back pain. They offer powerful, evidence-based ways to get to the source of your discomfort, helping you get your mobility back and return to living a life with far less pain.
When you're dealing with back pain day in and day out, questions are going to come up. It's only natural. You might wonder if you're on the right track, if a certain twinge is normal, or when you should start expecting real results. Getting solid answers to these questions is a huge part of taking back control.
Let's dive into some of the most common things people ask when they're figuring out how to manage chronic back pain. I'll give you the straight-up, practical answers you need.
This is probably the number one question I hear, and it’s a fair one. While a gentle stretch might offer a moment of relief right away, the real, lasting change that comes from a targeted exercise program is a long game. We're talking weeks, not days.
For most people, it takes a consistent effort for about 6 to 8 weeks to notice a meaningful drop in pain and a real improvement in how they move. The key word there is consistent. You're not just trying to soothe today's ache; you're building a stronger, more resilient back that can support you for years.
A Quick Reality Check: Your progress won't be a perfect, straight line. You'll have good days and bad days. That's completely normal. The goal is to see an overall trend of more good days and less pain over several weeks. A temporary flare-up doesn't mean you've failed.
The old heat-versus-ice debate can be confusing, but I'll simplify it for you. When you’re dealing with that persistent, nagging chronic back pain, heat is almost always your best friend. A heating pad or a warm bath can feel like a miracle worker, and there's good science behind it.
So, where does ice fit in? Think of ice for fresh, acute injuries—like if you just tweaked your back lifting something heavy. It's great for the first 48 hours to reduce swelling and numb that sharp, immediate pain. But listen to your body. Some people swear by alternating between the two, so don't be afraid to experiment and see what gives you the most relief.
Yes, one hundred percent. The food you eat has a massive, and often overlooked, impact on your body's inflammation levels. Imagine your pain is a smoldering fire. Eating a lot of sugar, processed junk, and unhealthy fats is like pouring gasoline on it.
On the flip side, shifting to an anti-inflammatory diet can help cool things down from the inside. It’s not about a crazy restrictive diet, but rather a focus on whole foods.
And don't forget to drink water! Your spinal discs are mostly water, and staying hydrated helps keep them spongy and effective at absorbing shock. It's a simple thing that makes a big difference.
It’s time to look beyond the basics when you’ve given conservative care an honest try. If you've been diligent with physical therapy, home exercises, and lifestyle adjustments for a few months and you're still stuck, it's a sign you need to explore other options.
If you're still battling debilitating pain, or if you have that relentless numbness or tingling from something like a herniated disc or sciatica, it’s definitely time to consult with a specialist. They can see if you're a good fit for powerful non-surgical therapies like spinal decompression that can address the root of the problem.
At Bonesetters Critical Chiropractic, our focus is on finding the true source of your pain and using advanced, non-surgical solutions to provide relief that actually lasts. If you're tired of temporary fixes and ready to get your life back, learn more about our evidence-based treatments at https://bonesetters.org.