Yes, neuropathy can absolutely improve, and in some cases, it can go away entirely. The key, however, lies in what's causing it in the first place.
If the nerve damage is tied to something fixable—like a vitamin deficiency or a temporarily pinched nerve—the outlook is often very positive once that root issue is resolved. But for neuropathy caused by a long-term, chronic condition, the focus usually shifts from a complete cure to effective, ongoing management.

If you're dealing with that frustrating tingling, numbness, or burning pain, the first question on your mind is probably, "Will this ever go away?" For many people, the answer is a hopeful yes. It all comes down to recognizing that neuropathy isn't a disease itself, but rather a signal that something else is wrong.
Think of neuropathy as a check engine light in your car. The light itself isn't the problem; it’s a warning that points to an issue with the engine. You wouldn't just cover the light with tape and keep driving—you'd get a mechanic to find and fix the underlying cause. It’s the same with neuropathy. The most effective treatment plans focus on diagnosing and addressing the source of the nerve damage.
To get a clearer picture of your recovery potential, it helps to group the causes into two main buckets: those that are often reversible and those that are chronic.
Reversible Causes: These are situations where, once you fix the problem, your nerves have a real chance to heal and regenerate. Common examples include vitamin B12 deficiencies, side effects from certain medications, or a pinched nerve from something like a herniated disc.
Chronic Causes: These involve ongoing health conditions that require consistent management. The goal here is to stop the nerve damage from getting worse and to keep symptoms under control. Advanced diabetic neuropathy is a perfect example of this.
The statistics really drive this point home. Studies looking at peripheral neuropathy treatment have shown that 83% of patients saw improvement in at least one symptom when they received the right care. For diabetic neuropathy specifically, 86% of patients found success with their treatment after one year. That number dropped to 55% after five years, which just underscores how crucial long-term management is for chronic conditions.
The road to feeling better is unique for everyone, but we see clear patterns based on what's causing the nerve issues. This table offers a quick snapshot to help you understand where your condition might fall.
| Neuropathy Cause | Potential for Recovery | Key Factors for Improvement |
|---|---|---|
| Vitamin Deficiency | High (Often Reversible) | Correcting the specific deficiency (e.g., B12, B6) through diet or supplements. |
| Nerve Compression | High (Often Reversible) | Relieving pressure on the nerve through therapies like spinal decompression. |
| Diabetes (Early Stage) | Moderate to High | Strict blood sugar control, lifestyle changes, and targeted therapies. |
| Medication-Induced | High (Often Reversible) | Discontinuing or changing the medication under a doctor's guidance. |
| Diabetes (Advanced) | Low (Focus on Management) | Preventing progression, managing symptoms, and improving quality of life. |
| Autoimmune Disorders | Variable (Focus on Management) | Managing the underlying autoimmune condition to reduce nerve inflammation. |
Ultimately, understanding the "why" behind your neuropathy is the first and most critical step toward finding relief. For a deeper dive into the different approaches available, check out our comprehensive guide to peripheral neuropathy treatment options.
To really get a handle on whether neuropathy can go away, we first need to look at what’s going on inside your body. The best way to think about your nervous system is like the intricate electrical wiring of a house. This network carries messages from the central hub—your brain and spinal cord—out to every part of your body, from your hands and feet to your internal organs.

Neuropathy is what happens when that wiring gets damaged. The protective insulation around the nerves, known as the myelin sheath, can get worn down, or the delicate fibers inside can fray. When that happens, the electrical signals traveling along those nerves get scrambled. Instead of a crisp, clear message, the signal might become weak, garbled, or even fire off at random.
This signal disruption is what you feel as symptoms. A weak or failing signal can cause numbness or that heavy, lead-like feeling in your limbs. Garbled, chaotic signals often translate into tingling or that classic "pins and needles" sensation. And when a nerve misfires completely, it can trigger sharp, burning, or shooting pains that seem to come out of nowhere.
Just like a house has different electrical circuits, your nervous system is divided into distinct networks. The type of neuropathy you experience depends entirely on which circuit has been compromised. Figuring this out is the first step toward effective treatment.
There are three main categories of neuropathy, each affecting a different part of your body's wiring:
Peripheral Neuropathy: By far the most common type, this affects the nerves that branch out from the brain and spinal cord to your arms, legs, hands, and feet. It's like damage to the wires running to the rooms farthest from the main circuit breaker. This is precisely why symptoms so often begin in the hands and feet.
Autonomic Neuropathy: This type impacts the nerves that manage your body's automatic functions—all the things you don't consciously control. Think of it as the wiring for your home's HVAC, plumbing, and security system. It regulates critical functions like your heart rate, blood pressure, digestion, and bladder control.
Focal Neuropathy: This involves damage to a single nerve or a specific cluster of nerves in one area. It's like a short circuit in the wire leading to just one appliance. Classic examples include carpal tunnel syndrome, which affects a nerve in the wrist, or Bell's palsy, which involves a facial nerve.
The key takeaway is this: neuropathy isn't the disease itself, but a symptom of nerve interference. Your body is sending a clear warning that its communication lines are down. The goal of any real treatment shouldn't be to just silence these signals with medication, but to find where the wiring is faulty and restore the connection.
Nerve damage rarely just happens on its own. It's almost always a downstream effect of another stressor or condition putting pressure on the system. Sometimes the damage is mechanical—think of a herniated disc physically pinching a nerve, literally squeezing the wire.
Other times, the cause is metabolic. Conditions like diabetes, for instance, can lead to high blood sugar, creating a toxic internal environment that slowly eats away at the nerve endings over many years. In other cases, autoimmune disorders can cause the body to mistakenly attack its own nerve tissues, leading to widespread inflammation and damage.
Understanding that neuropathy is a consequence of an underlying problem is a game-changer. It shifts the entire conversation. Instead of just asking, "Does neuropathy ever go away?" we can start asking a far more productive question: "What's causing the nerve damage, and how can we remove that interference so the body can finally begin to heal itself?" This simple reframing is the first real step toward finding a lasting solution.
When we talk about whether neuropathy can go away, we’re really asking about two very different scenarios: one where the damage is reversible, and one where it's chronic. The deciding factor, almost every time, is the root cause of the nerve damage.
Think of it like a wilting plant. If it’s just thirsty, a good watering can bring it right back to life. But if the soil itself is poisoned, the plant is going to be in trouble for the long haul. Your nerves are surprisingly similar. When we can find and remove the source of the problem, your nerves have a fantastic ability to heal. But if the cause is a deep-seated, ongoing issue, our focus has to shift from a cure to smart, proactive management.
Figuring out which path you're on is the first and most important step. It sets realistic expectations and helps us build a treatment plan that actually works.
The good news is that many cases of neuropathy are, in fact, reversible. This happens when there's a clear, identifiable problem that we can fix. Once that source of irritation is gone, the body's incredible healing mechanisms can get to work repairing the nerve.
This is more common than you might think. We see it all the time with specific, correctable issues.
For instance, a patient came to us with severe numbness and tingling in his foot that made walking a real challenge. After a thorough exam, we found the problem wasn't in his foot at all. It was a compressed nerve in his lower back from a bulging disc. We started him on a course of targeted spinal decompression therapy, which gently relieved that pressure. Before long, the nerve signals to his foot were restored, and the numbness vanished.
This is a perfect illustration of reversible neuropathy. We simply removed the physical roadblock, and the nerve knew exactly what to do to heal itself.
On the flip side, chronic neuropathy stems from nerve damage caused by a long-term condition that we can't just "turn off." In these cases, the source of the damage is persistent, so the game plan changes. The goal shifts from complete reversal to aggressive management. We aim to halt the progression of the damage, manage symptoms to improve your quality of life, and support your overall nerve health as much as humanly possible.
Some of the most common causes of chronic neuropathy include:
Even when the damage is chronic, it's not a life sentence of misery. Far from it. An effective management strategy can make a huge difference. The focus becomes a team effort: stabilizing the underlying disease, using therapies to calm inflammation and boost circulation, and adopting lifestyle habits that give your nerves the best possible support.
While a total cure might not be on the table, achieving a significant improvement in your symptoms and daily function is a very realistic and worthy goal.
Getting to the bottom of nerve pain is a bit like being a detective. To figure out if your neuropathy can go away, we have to trace the symptoms back to their source. Just treating the pain is like repeatedly hitting the snooze button on a fire alarm without ever looking for the fire. It doesn't solve the underlying problem.
Our process starts with a simple conversation. We listen to your story—your full medical history, how the symptoms started, and how they impact your life. This isn't just background noise; it's where we find the first critical clues that guide our entire investigation.
Next, we roll up our sleeves for a thorough physical and neurological exam. We'll check your reflexes, test muscle strength, and map out your sensory responses. This hands-on assessment shows us exactly which nerves are struggling and helps us pinpoint the location of the interference, which is often nowhere near where you actually feel the pain.
It’s surprisingly common for tingling in the hands to be caused by a pinched nerve in the neck, or for foot numbness to originate from an issue in the lower back. Think of it like a kink in a garden hose. The water stops coming out of the nozzle, but the actual problem is much further up the line. This is precisely why we look at the entire system, not just the area that hurts.
This flowchart shows how different causes of neuropathy lead down two distinct paths: one toward potential recovery and the other toward managing a chronic condition.
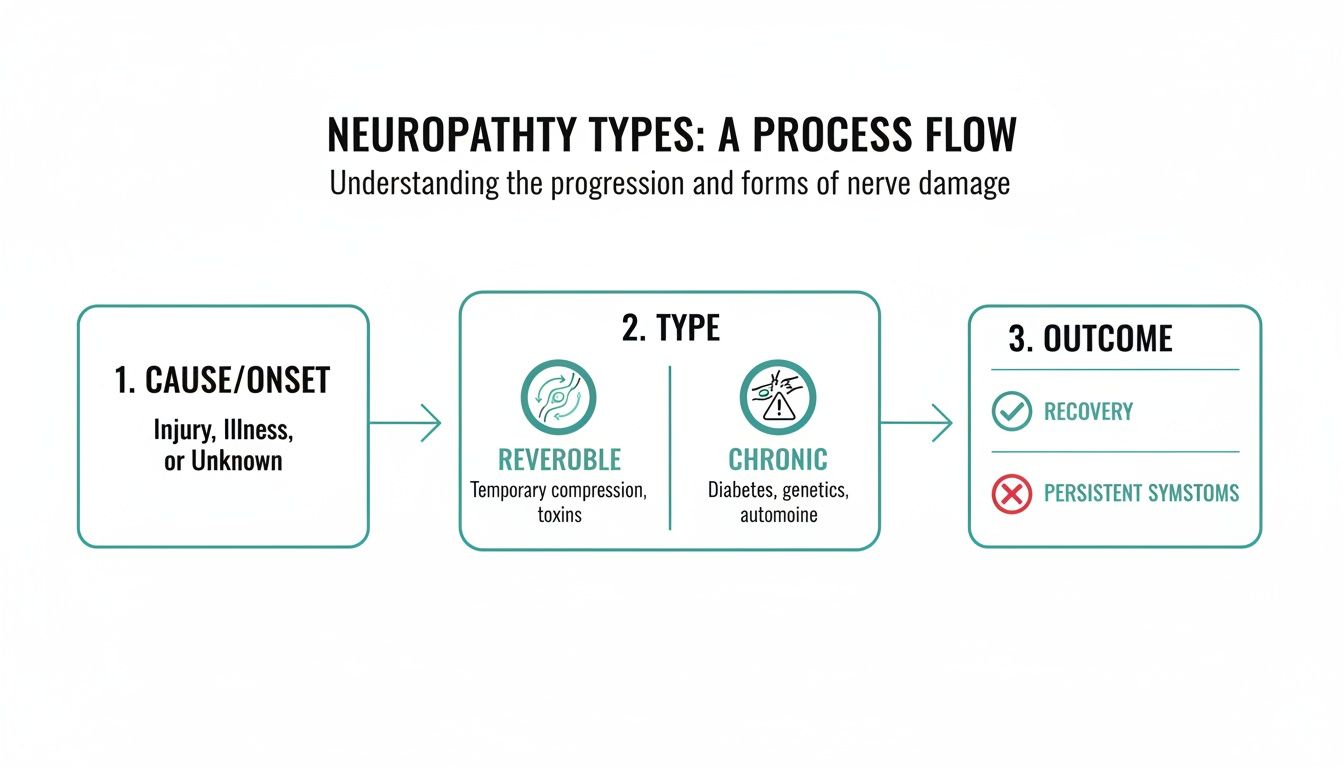
Ultimately, our diagnostic process is all about determining which path you're on. This ensures your treatment plan is perfectly aligned with the root cause of your symptoms from day one.
Sometimes, a physical exam isn't enough to get the full picture. When we need to see exactly what’s happening inside your body, we turn to advanced diagnostic tools. These aren't just for confirming a diagnosis; they're for understanding the why and the where with total clarity.
A precise, evidence-based diagnosis is the roadmap that guides every step of your recovery plan. It ensures we are treating the root cause of your pain, not just chasing the symptoms. This is the difference between temporary relief and a plan for lasting recovery.
Here are some of the tools we might use to get those answers:
By combining your personal story, a detailed physical exam, and these targeted tests, we build a complete and accurate picture of what's going on. This crucial first step takes the guesswork out of your pain and gives us a solid, reliable strategy to help you move forward.
Once we’ve pinpointed the root cause of your nerve pain, the next logical step is to create an environment where the nerves can actually heal. This isn’t about masking symptoms with medication. Instead, modern non-surgical treatments focus on correcting the underlying mechanical and physiological problems—and that’s often the key to determining if neuropathy can go away for good.

The whole approach is built around fostering nerve regeneration. We do this by improving circulation, taming inflammation, and taking off the physical pressure that scrambles nerve signals in the first place. These therapies are designed to create the ideal conditions for your body's own natural healing processes to take over.
For so many people, the neuropathy they feel in their hands or feet actually starts from a compressed nerve in the spine. Think of it like standing on a garden hose—the problem isn't the nozzle, it's where the pressure is being applied. Spinal Decompression Therapy gets right to the source by creating negative pressure around the spinal discs.
This gentle, targeted force helps draw back bulging or herniated discs, taking that direct pressure off the pinched nerve roots. Once the pressure is off, blood flow, oxygen, and vital nutrients can flood the area again. This kickstarts the healing process and allows clear signals to finally travel down the nerve pathway.
Restoring proper function is about more than just pain relief; it's about giving the nerve a fighting chance to repair itself. When the interference is removed, the body has a remarkable capacity for recovery.
Even in serious medical situations, the potential for nerve recovery is significant. For instance, in neuropathy linked to critical illness, studies have found that 70.3% of patients achieve a full recovery. And with longer-term follow-up, that number climbs to an impressive 88.8%. It really highlights the body’s resilience when given the right support.
Another powerful tool we have for nerve healing is Class IV Cold Laser Therapy. This technology uses specific wavelengths of light energy that penetrate deep into your tissue without creating any heat. Damaged cells absorb this light energy, which essentially gives a jolt to their mitochondria—the "powerhouses" of the cell.
This stimulation kicks off a chain reaction of positive effects:
In short, the therapy gives your damaged nerves a much-needed energy boost, helping them repair faster and function better. You can learn more by exploring our guide on https://bonesetters.org/cold-laser-therapy/.
Real, lasting nerve healing rarely comes from just one treatment. The most effective strategies combine several different methods to attack the problem from all sides, creating a synergistic effect that leads to lasting relief.
Other supportive therapies can include:
In some situations, neuropathy is tied to an underlying infection or condition that needs a much broader treatment strategy. For example, looking into supportive options like hyperbaric treatment for Lyme disease could offer complementary benefits for nerve healing in certain people. By combining these advanced, non-surgical tools, we can build a comprehensive plan that doesn’t just manage symptoms but actively helps your body heal its damaged nerves.
Professional treatments are fantastic for tackling the root cause of nerve pain, but it's your daily habits that truly make or break long-term healing. Think of it as a partnership. While your doctor provides the game plan and the advanced tools, you’re the one on the field every single day, making the choices that move the needle.
Taking an active role is about more than just following instructions; it’s about taking control. It’s a shift from just receiving care to actively participating in your own health. The small, consistent things you do create an internal environment where your nerves can actually heal and stay protected for the long haul.
The food you eat is literally the raw material your body uses to repair itself. Adopting an anti-inflammatory diet is one of the most powerful things you can do for your recovery. This isn't about a fad diet; it's about focusing on whole, nutrient-rich foods that fight inflammation and give your nerves the building blocks they need.
At the same time, you have to cut out the things that work against you. Processed foods, sugary drinks, and refined carbs create a toxic, inflammatory environment that makes it nearly impossible for your nerves to heal.
If you have diabetic neuropathy, this is the big one. Getting your blood sugar under control is the single most important thing you can do to stop nerve damage in its tracks. High blood sugar is poison to your nerve endings, and no therapy in the world can outrun uncontrolled glucose levels. For anyone with prediabetes or diabetes, learning how to lower A1C naturally with your doctor's approval is a critical piece of the healing puzzle.
Don't underestimate how much this matters. Just look at a condition like Chronic Inflammatory Demyelinating Polyneuropathy (CIDP), an autoimmune disorder. With the right treatment, research shows that approximately 90% of patients improve. A five-year study found that 87% of patients were still able to walk, and a remarkable 26% achieved complete remission—needing no treatment for over two years. That’s the power of a dedicated approach.
I get it. When you’re in pain, exercise is probably the last thing on your mind. But gentle movement is absolutely essential for nerve health. It gets your blood flowing, delivering a fresh supply of oxygen and nutrients to damaged nerves while helping to clear out metabolic junk.
Consistent, mindful movement doesn't just improve physical strength; it enhances the communication between your brain and your body, which is at the very heart of nerve recovery.
You don't need to run a marathon. Simple, low-impact exercises can make a huge difference. Things like walking, swimming, or tai chi are perfect for improving balance, reducing stiffness, and helping to manage pain. The goal is just to stay active in a way that feels good and supports your body's healing journey.
As you start to tackle nerve pain, it's completely normal for questions to pop up. Getting a handle on how nerves heal can give you the confidence you need to stick with your recovery plan. Let's walk through some of the most common questions we hear from patients.
Nerve healing is a marathon, not a sprint. There's no single timeline, as it really depends on what caused the damage and how severe it is. If the issue was something straightforward like a vitamin deficiency, you could start feeling better within a few weeks to months after correcting it.
But for more serious damage from an injury or long-term compression, the body has to work a lot harder. Nerves regenerate at a snail's pace—roughly one inch per month. This means recovery can take a while, but it absolutely can happen. The most important thing you can do is stay consistent with your treatment and lifestyle adjustments to give your nerves the best possible chance to mend.
This is a big one. While significant, long-standing diabetic neuropathy isn't something we can typically "reverse" in the traditional sense, we can absolutely stop it from getting worse and make a huge dent in the symptoms. The single most powerful tool here is tight control of your blood sugar. Once you get that stabilized, you stop feeding the fire that's damaging the nerves.
When you combine excellent blood sugar management with therapies designed to boost circulation and improve nerve signaling, the results can be remarkable. Many patients see their pain, tingling, and numbness fade dramatically, letting them get back to the life they want to live. The goal shifts from a "cure" to profound symptom relief and active management.
A quick heads-up: it's very common for symptoms to come and go during the healing process. You'll likely have good days and bad days. Sometimes, as nerves start "waking up," you might even feel new or strange sensations. This is often a great sign that the lines of communication are being reconnected.
The early signs of nerve healing can be easy to miss, so you have to become a bit of a detective. Often, the first thing people notice is that their worst symptoms start to back off—the sharp, shooting, or burning pains that really interfere with life begin to quiet down.
Other positive signs to watch for include:
Any positive shift, no matter how small it seems, is a huge sign that your body is responding and your treatment is on the right track. Keeping a simple log of these little victories can be a fantastic way to stay motivated. Remember, every step forward is a win.
At Bonesetters Critical Chiropractic, we focus on digging deep to find the root cause of your nerve pain. From there, we build a personalized, non-surgical plan aimed at true, lasting healing. If you’re done with just masking symptoms and want a real solution, we're here to help.
Take the first step toward getting your life back. Discover how our evidence-based therapies can restore your comfort and mobility. Schedule your comprehensive consultation today at Bonesetters.org.