When your doctor says "knee replacement," it's easy to think your options have run out. But I'm here to tell you that for most people, surgery isn't the starting line—it's the final resort. There's a whole world of effective alternatives to knee replacement surgery that can get you moving again, reduce your pain, and potentially keep you out of the operating room altogether.
Let's walk through the path of non-surgical care, giving you the knowledge you need to take control of your knee health.
The idea that you can manage severe knee pain without going under the knife isn't just wishful thinking; it's a reality for a huge number of patients. The healthcare landscape is actively shifting to support these non-operative treatments. Why? The numbers tell the story. The global market for knee replacements is expected to balloon to nearly $17.8 billion by 2034. This incredible demand, fueled by an aging population and more osteoarthritis diagnoses, gives us a powerful reason to find better ways to help people before surgery becomes the only answer.

To help you see the full picture, here's a quick breakdown of the main non-surgical strategies we'll be exploring. Think of it as a menu of options we can combine to create your ideal treatment plan.
| Alternative Category | Primary Goal | Ideal Candidate Profile |
|---|---|---|
| Conservative Care | Build a strong foundation for knee health by reducing load and improving support. | Anyone with mild to moderate knee pain, especially if overweight or new to treatment. |
| Pain Management | Directly target and reduce inflammation and pain signals to improve daily function. | Individuals experiencing flare-ups or persistent pain that limits activity. |
| Injections & Regenerative | Deliver targeted relief directly into the joint to lubricate, reduce inflammation, or stimulate healing. | Those with moderate to severe arthritis who need more than conservative care. |
| Advanced Therapies | Use modern technology to promote tissue repair and restore healthy joint mechanics. | People with chronic, stubborn knee pain who haven't found relief with other methods. |
This table gives you a bird's-eye view, but the real power comes from understanding how these tools work together. Let's dive a little deeper.
The first step to avoiding surgery is knowing what’s in your toolbox. These alternatives aren't just temporary fixes; they are powerful, proven strategies that get to the root of what’s causing your knee pain.
We can organize these tools into a few key categories:
The goal is to build a personalized treatment plan that layers these strategies effectively. By starting with the least invasive options and progressing as needed, you create the best possible opportunity to manage your knee health for the long term and avoid the operating room.
Before we even start talking about advanced procedures, it’s crucial to understand that the most powerful alternatives to knee replacement often begin with simple, fundamental changes. Think of it as building a better support system for your knee joint from the ground up.
This isn't a "wait and see" approach. Conservative care is an active strategy, backed by solid evidence, designed to get you moving better, reduce your pain, and genuinely change the trajectory of your knee arthritis for the better.

The core idea is simple: take the load off the joint while making it more stable. This two-pronged attack forms the bedrock of any successful non-surgical plan. When you commit to this foundation, the relief can be significant and long-lasting, drastically improving your day-to-day life.
One of the single most impactful things you can do for your knees is manage your weight. The physics of it are staggering. Research has shown time and again that for every one pound of weight you lose, you take four pounds of pressure off your knees when you walk.
Let that sink in. This "force-multiplier" effect is a complete game-changer. Losing just 10 pounds is like taking a 40-pound pack off your back every single time you take a step. This isn't just about easing pain; it slows down the grinding wear-and-tear that drives arthritis, giving the joint some much-needed breathing room.
A weight reduction of just 5-10% of your total body weight can lead to a significant decrease in knee pain and a noticeable improvement in your ability to move. For a 200-pound individual, that’s a loss of only 10-20 pounds to achieve meaningful results.
If weight loss is about reducing the load, physical therapy is all about building up the support structure. A common myth is that you shouldn't exercise an arthritic knee for fear of making it worse. The truth is, the right kind of movement isn't just helpful—it's absolutely essential.
A good physical therapist is like an architect for your body. They design a personalized plan to beef up the key muscles—quadriceps, hamstrings, and glutes—that act as your body’s natural shock absorbers. When these muscles are strong, they take the stress of daily movement so your cartilage doesn’t have to.
This specialized therapy usually includes:
Beyond the exercises, many therapists use other methods to get you better, faster. For example, they might use special tools to release tight fascia and break down scar tissue. You can learn more about how practitioners use these techniques in our guide on Instrument Assisted Soft Tissue Mobilization. It's this comprehensive approach that truly helps restore how your knee is supposed to work.
Finally, laying a strong foundation means making smarter choices in your daily life. This isn't about giving up the activities you love, but rather finding better ways to do them. It's about working with your body instead of fighting against it.
Simple tweaks can make a world of difference:
When you combine these three pillars—weight management, targeted physical therapy, and smart daily habits—you create a powerful effect. You're actively reducing the forces that cause damage while building a stronger, more resilient knee. This is always the most important first step on the path to finding relief without surgery.
So, you've tried physical therapy, exercise, and other conservative approaches, but the knee pain just isn't letting up. What's next? Before jumping to surgery, it's worth exploring treatments that work directly inside the joint itself. Injection-based therapies can be a powerful next step, offering a more targeted way to manage pain, reduce inflammation, and improve how your knee functions.
It's important to remember, though, that these aren't a one-size-fits-all fix. Each type of injection has a different job to do, a different timeline for relief, and works best for different people. Understanding what makes them tick is key to figuring out the right path forward for you.

Think of a corticosteroid injection as the fire department for an angry, inflamed knee. Its main purpose is to show up fast and put out the fire—that is, the intense inflammation driving your pain and swelling. When you're in the middle of a bad flare-up, a steroid shot can feel like a miracle, often bringing significant relief within just a few days.
This quick action makes corticosteroids a fantastic tool for getting a handle on acute pain. But it's best to see them as a temporary fix, not a long-term solution. The relief usually lasts for a few weeks or maybe a couple of months, and using them too often can lead to diminishing returns and potential side effects.
If steroid shots are firefighters, think of hyaluronic acid (HA) injections as giving your knee a much-needed oil change. Your joints naturally contain hyaluronic acid, a slick, viscous substance that helps lubricate the cartilage and absorb shock. In an arthritic knee, this natural lubricant breaks down and thins out, leading to that grinding, bone-on-bone feeling.
HA injections, often called "gel shots," are designed to supplement your body's depleted supply. The goal is to restore that smooth, gliding motion and reduce the friction that causes pain.
Corticosteroids offer a quick but temporary fix for inflammation. Hyaluronic acid, on the other hand, is a longer-term play aimed at improving the very mechanics of how your knee joint moves.
Going beyond just managing symptoms, a newer class of treatments aims to fundamentally change the environment inside your knee for the better. This is the whole idea behind regenerative medicine—using your body’s own powerful healing components to fight inflammation and create healthier conditions for your existing tissues.
You can think of it like gardening. Instead of just pulling the weeds (reducing inflammation), regenerative therapies work to fertilize the soil, helping create a more resilient and healthier garden overall. The two big players in this field are Platelet-Rich Plasma (PRP) and cell-based therapies.
Platelet-Rich Plasma (PRP) Therapy
PRP therapy begins with a simple blood draw from your arm. That blood is then spun in a centrifuge to separate and concentrate the platelets—tiny but mighty cell fragments packed with growth factors. This concentrated, golden liquid is then carefully injected back into your knee.
These growth factors are like little biological instruction manuals, signaling your body to:
While PRP won't regrow a new layer of cartilage, by dramatically improving the joint's internal environment, it can lead to major reductions in pain and improvements in function that can last for a year or even longer.
Cell-Based Therapies
Often called "stem cell" treatments, cell-based therapies take this concept even further. These highly potent cells are typically harvested from your own body (usually from fat tissue or bone marrow) and, like PRP, are injected into the knee. While their potential is enormous, research is still ongoing to fine-tune their use and determine who they help the most.
The effectiveness of these injections really varies from person to person. Corticosteroids provide fast, short-term relief for most, while HA can offer a longer runway of comfort for up to six months. Regenerative options like PRP are showing incredible promise, though results can differ. Fortunately, ongoing studies are helping us pinpoint which patients will get the most benefit.
You can explore a summary of the research on these non-surgical pathways, which are widely used to defer the need for surgery. We encourage you to read the full research about these alternatives and their outcomes.
When the standard approaches and injections just aren't cutting it, it’s easy to think surgery is your last and only resort. But that's not always the case. A new wave of powerful, non-invasive therapies is changing the game by targeting the root causes of knee pain, offering real relief and restoring function without ever making an incision. These advanced treatments use smart technology to create the perfect healing environment right inside the knee.
Think of a knee with arthritis as a room where everything has gone wrong. The pressure is too high, the air is stale, and the electrical wiring is on the fritz. These modern therapies work together to fix each problem. They gently open up space, improve circulation to bring in fresh nutrients, and reset nerve signals to dial down the pain. It’s this integrated approach that makes it such a strong alternative to knee replacement for so many people.
Picture your knee joint as a sponge that’s been squeezed dry. When cartilage thins out and the joint space shrinks, that’s essentially what happens. The constant pressure chokes off the flow of healing fluids and vital nutrients, which only makes the joint break down faster and hurt more.
Knee decompression therapy is designed to reverse that. The system applies a gentle, rhythmic pull that carefully separates the bones of the knee joint. This creates negative pressure—almost like a subtle vacuum—that pulls oxygen, hydration, and nutrient-rich fluid back into the joint. It’s like slowly releasing that compressed sponge and allowing it to soak up nourishment again.
Over a series of treatments, this process helps to:
By creating space and getting fluids moving, decompression can lead to significant pain relief and better mobility.
Once we’ve created some space with decompression, the next step is to kickstart the repair process at the cellular level. That’s where Class IV cold laser therapy comes in. Don't worry, this isn't a laser that cuts or burns. Instead, it uses specific wavelengths of light that penetrate deep into your knee tissue.
This process is called photobiomodulation, and you can think of it as giving your cells a high-energy pep talk. The light is absorbed by the mitochondria—the tiny powerhouses inside your cells—and supercharges them. This triggers a chain reaction of positive effects:
This surge in cellular activity speeds up your body's own natural healing mechanisms, resulting in faster tissue repair and a noticeable drop in pain. It’s a direct attack on the inflammation and damage that fuel arthritis.
Finally, we have to fix the communication breakdown between your nerves and muscles. Chronic knee pain makes muscles weak and causes nerve signals to go haywire, which leads to instability and poor movement patterns that just make things worse.
Horizontal Stimulation is a sophisticated form of electrical therapy that goes far beyond a typical TENS unit you might buy at a store. It sends calming, healing frequencies deep into the tissue to help reset nerve pathways and soothe spasming muscles. It’s like re-tuning a radio station from fuzzy static to a crystal-clear signal.
We often pair this with targeted chiropractic adjustments, which focus on getting the knee and surrounding joints moving in proper alignment again. When the knee is moving correctly and nerve communication is restored, we can finally break the cycle of pain and dysfunction. These therapies are frequently used alongside other tools, and you can see how different modalities work together by reading our guide explaining what therapeutic ultrasound is.
By combining knee decompression, laser therapy, and advanced stimulation, we create a complete healing strategy. This multi-pronged attack addresses pain from every angle—mechanical, cellular, and neurological—offering a powerful, cohesive alternative for anyone looking for lasting relief from chronic knee pain.
With so many non-surgical knee treatments available, it's easy to feel a bit lost. How do you know which one is right? The most important thing to remember is that there’s no magic bullet—the “best” treatment is always the one that’s best for your specific situation.
Making that choice isn't something you do alone. It's a conversation between you and your doctor, and it really comes down to a few key things: how severe your knee arthritis is, your age, what you want to be able to do, and your overall health. A treatment that’s perfect for a 45-year-old training for a half-marathon might be completely different from what a 70-year-old who wants to garden pain-free needs.
Think of your options as being on a spectrum. At one end, you have foundational approaches like physical therapy and weight management, which are a great starting point for almost everyone. At the other end, you'll find more advanced therapies designed for stubborn, long-term pain that hasn't responded to the basics.
The condition of your joint is a huge piece of the puzzle. If your X-rays show you still have some cartilage left—a decent amount of joint space—then regenerative options like PRP could be a game-changer. But if your knee has reached a "bone-on-bone" stage, the focus might shift to treatments that manage symptoms and improve how the joint functions.
Your goals are just as critical. Are you hoping to get back to playing tennis, or is your main goal simply to walk through the grocery store without that nagging ache? Being crystal clear about what a “win” looks like for you is the best way to zero in on the right alternatives.
The flowchart below gives you a sense of how some of the more advanced non-surgical treatments fit together to tackle knee pain from different angles.
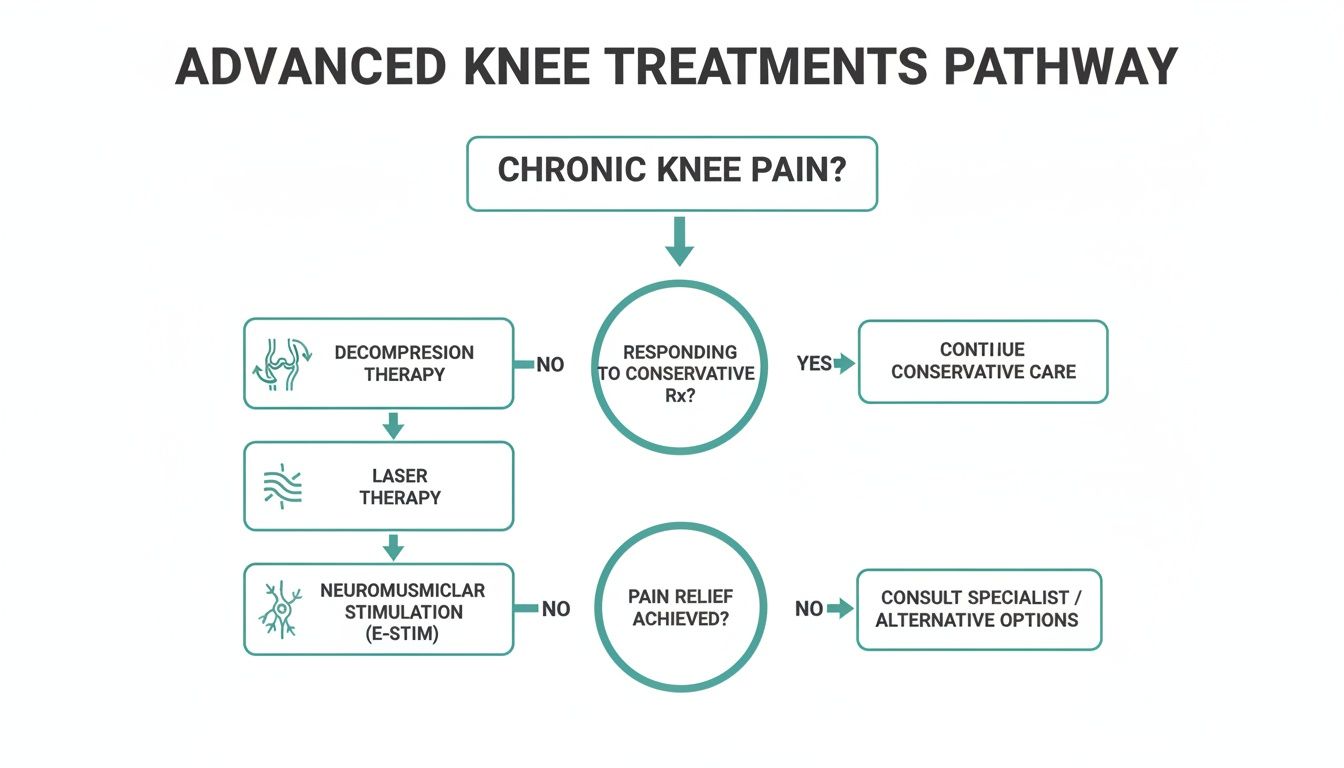
As you can see, a comprehensive plan might use decompression to address mechanical stress, laser therapy to promote healing at a cellular level, and stimulation to calm down overactive nerves. It's all connected.
To help you get a clearer picture of how these treatments stack up, here is a simple comparison table. This is just a general guide, as everyone's experience will be a bit different.
| Treatment Option | Best For (Severity) | Typical Time to Relief | Duration of Benefits | Invasiveness Level |
|---|---|---|---|---|
| Physical Therapy & Exercise | Mild to Moderate | 4-8 weeks | Ongoing with consistency | Non-Invasive |
| Bracing & Orthotics | Mild to Moderate | Immediate | As long as worn | Non-Invasive |
| Pain Medications (NSAIDs) | Mild to Moderate | Within hours | Short-term (hours) | Minimal |
| Corticosteroid Injections | Moderate to Severe | Days to 1 week | 3-6 months | Minimally Invasive |
| Hyaluronic Acid Injections | Mild to Moderate | 4-6 weeks | 6 months or more | Minimally Invasive |
| PRP & Regenerative Therapies | Mild to Moderate | 1-3 months | 1 year or more | Minimally Invasive |
| Advanced Non-Surgical Program | Moderate to Severe | 2-4 weeks | Long-term, potentially permanent | Non-Invasive |
This table highlights how different approaches are suited for different stages of knee pain and offer varying timelines for relief. It’s a great starting point for your discussion with a healthcare professional.
Choosing an effective non-surgical path isn't just a personal win—it has ripple effects across the entire healthcare system. Knee replacement is a massive industry, with a global market projected to reach tens of billions of dollars.
Finding ways to help people avoid or delay surgery, even by a small percentage, can lead to huge cost savings for everyone. That’s why many health systems are putting more resources into conservative care programs. By helping a younger patient postpone their first knee replacement by even 5–10 years, these programs can dramatically reduce the odds they'll need a more complicated and expensive revision surgery later in life. You can explore more about the economic drivers of non-surgical care and see how they're shaping the future of treatment.
The most successful treatment plans are personalized and dynamic. They start with the least invasive options and adapt as your needs change, always with the goal of restoring function and improving your quality of life.
Ultimately, this is a shared decision. The more you know about your options and the more honest you are about your goals, the more productive your conversation with your doctor will be. That teamwork is the surest way to build a plan that gets you moving again and lets you live with less pain.
Look, this entire guide is about exploring the incredible world of non-surgical knee treatments, and for good reason—they work wonders for so many people. But it's just as important to be realistic. The goal isn't to avoid surgery at all costs; it's to avoid unnecessary surgery.
Sometimes, a knee replacement is absolutely the best path forward. Thinking about surgery isn’t a sign that other treatments failed. It’s simply recognizing that your knee has reached a point where a structural fix is needed to give you back the life you deserve.
So, how do you know you've reached that point? A few clear signs usually tell the story. If you're nodding along to any of these, it's probably a good time to have a serious conversation with a surgeon.
Here's what to watch for:
Let's be frank: if you've given it a real shot—you've done the physical therapy, you've tried the injections, and maybe even our advanced therapies—and you're still not getting any meaningful, long-term relief, that's a powerful message. It's your body telling you the underlying problem needs a different kind of solution.
Considering surgery at this stage isn't giving up. It's taking the next logical step to get your mobility, your independence, and your life back on track.
When you're facing a major decision about your knee health, you're bound to have questions. Let's tackle some of the most common ones we hear from patients who are looking for a path back to an active life without surgery.
This is probably the most common question we get, and the answer is: it depends. Insurance coverage can be a real mixed bag when it comes to non-surgical knee care.
Most insurance plans will readily cover the basics like physical therapy and standard anti-inflammatory medications (NSAIDs), though you'll likely have a copay or a cap on the number of PT sessions. When it comes to injections, corticosteroid shots are usually covered. Hyaluronic acid, or "gel shots," often require prior authorization, meaning your doctor has to prove to the insurance company that they're medically necessary for you.
Where things get tricky is with newer, more advanced options. Regenerative treatments like PRP and specialized therapies like knee decompression are frequently classified as "investigational" by insurers, which usually means they are not covered and would be an out-of-pocket expense. The best first step is always to call your insurance provider directly to understand your specific benefits.
Think of your first visit as a deep dive into the story of your knee. We’ll sit down and have a real conversation about your pain—when it started, what it feels like, and most importantly, how it's holding you back from doing the things you love. We'll also go over any treatments you’ve already tried.
Next comes a thorough physical exam where we'll check your knee’s range of motion, test its stability, and assess the strength of the surrounding muscles. We'll also review any recent X-rays to get a clear look at the joint itself, paying close attention to the amount of space between the bones. The entire goal is to build a complete, 360-degree picture of your situation so we can map out a treatment plan that actually makes sense for you.
Remember, your first appointment is a partnership. Be ready to ask your own questions about the diagnosis, why certain treatments are being recommended, and what you can realistically expect in terms of relief and timing.
Not only can you, but you absolutely should. The most effective non-surgical strategies rarely rely on a single treatment. A truly comprehensive plan attacks the problem from multiple angles at once, creating a combined effect that's far more powerful than any one therapy alone.
A successful plan might weave together several approaches, for example:
By addressing the mechanical stress, the biological inflammation, and the functional weakness all at once, you get a much better shot at lasting relief.
There isn’t a one-size-fits-all answer here, as every knee and every person is different. That said, with a consistent and well-managed non-surgical plan, you should start to notice a real, measurable difference within a few months.
The rule of thumb is to give it a fair shot. If you've been diligently following a plan for six to twelve months—combining several different conservative and advanced therapies—and your pain is still severe and your life is still limited, that’s the point where it might be time to have a serious conversation about surgical options. The goal is to exhaust these powerful alternatives first, giving them a genuine opportunity to help you heal.
Ready to see if a non-surgical plan can get you back on your feet? At Bonesetters, we specialize in creating personalized programs that combine proven therapies to restore mobility and help you avoid surgery. Find out more about our unique approach and book your initial consultation at https://bonesetters.org.