If you're struggling with a deep, nagging ache in your neck or low back, you're in good company. This is the classic signature of facet joint pain, a condition that can turn simple, everyday movements into a major chore. The most effective treatment for facet joint pain is always a thoughtful, step-by-step process—one that starts with simple, conservative care and only escalates to more advanced options if they're truly needed.
Imagine your facet joints as the small, stabilizing knuckles connecting your vertebrae. When they get irritated or inflamed, they can seriously disrupt your life. This guide is designed to be your roadmap back to comfort, walking you through the entire journey from figuring out what’s wrong to exploring treatments that can get you moving freely again.
Our goal here is to clear up the confusion and show you how a smart, targeted strategy can fix the underlying problem, often helping you sidestep surgery altogether.
Tackling facet joint pain effectively requires a bit of a mental shift. Instead of just chasing symptoms with quick fixes, the best outcomes come from focusing on restoring proper function and giving your body what it needs to heal itself. This means recognizing that relief is a process, not a single event.
A successful treatment plan is built on an accurate diagnosis and a progressive ladder of care. It’s about using the least invasive, most effective methods first to build a foundation for lasting recovery.
Think of it as a partnership between you and a specialist who actually listens. The plan should be designed for you—your body, your pain, and your lifestyle. It’s not about a one-size-fits-all fix, but a personalized strategy that adapts as you improve.
The path to relief is structured to be both gentle on your body and highly effective. We'll look at how different treatments build on each other, creating a complete system of care that ensures you get the right intervention at the right time.
The key stages in managing facet joint pain usually follow this logical order:
By following this progression, you can feel confident in your decisions. Each step is designed to give you the most benefit with the least risk, putting you in the driver's seat of your own recovery. This guide will give you the knowledge you need to find the right treatment for facet joint pain and get back to the active, comfortable life you deserve.
Figuring out if your back pain is coming from a facet joint isn't just about looking at an MRI. It’s more like good old-fashioned detective work, where a specialist pieces together clues from a few different sources to be absolutely sure they’ve found the right culprit.
This process is a journey, and it almost always stands on three core pillars: a hands-on physical exam, a look inside with advanced imaging, and a highly specific test called a diagnostic block to confirm our suspicions. Each step gives us a unique piece of the puzzle, making sure your treatment for facet joint pain is aimed at the right target from the very beginning.
Everything starts with a conversation and a hands-on assessment. A skilled clinician will want to understand your posture, check your reflexes, and see how well you move. They'll guide you through specific motions—like bending backward, leaning forward, or twisting side-to-side—to see exactly what makes the pain better or worse.
This part is vital because the way your pain behaves tells us a lot. For instance, if you have tenderness right over a specific joint in your spine, or if the pain flares up when you arch your back, that’s a classic sign pointing toward the facet joints. You can learn more about how specialists use touch and movement to zero in on problem areas in our guide on how chiropractors know where to adjust.
While the physical exam gives us clues, imaging lets us see what’s going on with the structures deep inside your spine. Tools like X-rays, CT scans, or an MRI are great for spotting signs of wear and tear, such as arthritis, bone spurs, or joints that have narrowed over time.
But here’s a crucial point: imaging alone can't give us the final answer. It’s surprisingly common for someone to have an MRI showing significant arthritic changes but feel perfectly fine. On the flip side, a joint can be screaming in pain without looking all that bad on a scan.
Imaging shows us the anatomy, but it doesn't always show us the pain. It’s a vital part of the picture, but it’s not the whole story. The next step is what truly confirms the diagnosis.
Once we have a clearer picture, we can start mapping out the best path forward, which this decision tree illustrates. It shows how we move from initial conservative care to more advanced options once the diagnosis is certain.
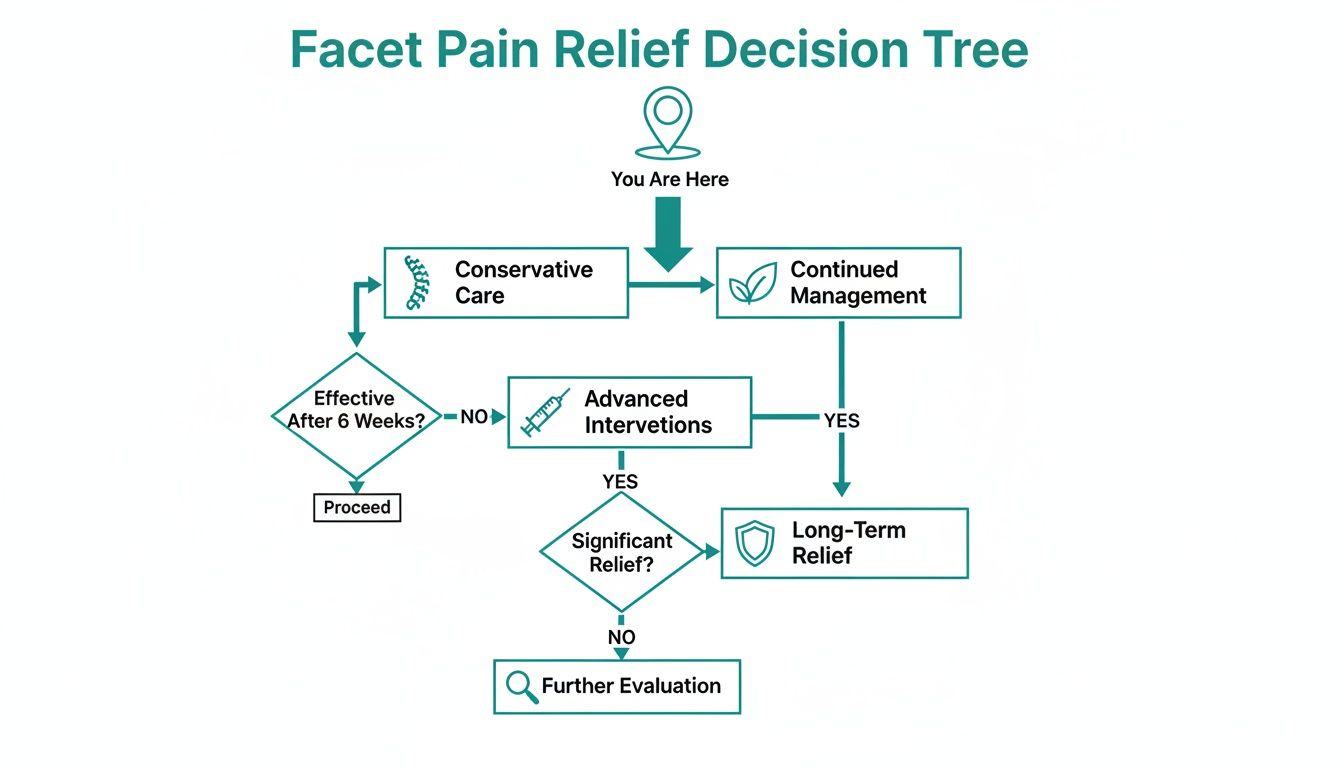
This structured approach ensures that our diagnostic work directly informs the treatment plan, giving you the best chance for real relief.
When it comes to definitively diagnosing facet joint pain, the gold standard is a procedure called a medial branch block. Think of it like flipping a circuit breaker in your house to see which light goes out. The medial branch nerves are the tiny "wires" that carry pain signals from the facet joints to the brain. If we can temporarily shut them off and the pain disappears, we've found our source.
Here’s how this highly precise procedure works:
Because a single injection can sometimes give a false positive, best practices often involve two separate blocks on different days. This careful approach helps confirm that the facet joint is the true culprit, especially since facet pain is a major player in chronic low back pain, accounting for 15% to 45% of cases. To be certain, guidelines recommend confirming the diagnosis with at least 50% to 90% pain relief that lasts for the expected duration of the anesthetic. This step is critical for ensuring that more definitive treatments, like radiofrequency ablation, are directed at the exact source of your pain.
For most people, the path to relief from facet joint pain starts with conservative, non-invasive treatments. You can think of this as building a solid foundation before you even think about putting up the walls of a house. These initial steps are all about calming down inflammation, getting you moving properly again, and strengthening the muscles that support your spine—all without needles or surgery.
This approach is so effective because it tackles the root mechanical issues that caused the pain in the first place. A smart treatment for facet joint pain always begins by giving your body the right tools to start healing itself.

Often, the very first step is the simplest: adjusting your daily routine to stop poking the bear. This doesn't mean you should stop moving entirely—that can actually make stiffness worse. It’s about making smart changes, like fixing your posture at your desk or learning how to lift things without putting a strain on your back.
Physical therapy takes this concept to the next level. A good therapist will create a personalized exercise plan to strengthen your core muscles. Think of these muscles as a natural corset that stabilizes your spine, taking the pressure off those irritated facet joints. The exercises are gentle but highly specific, zeroing in on the deep abdominal and back muscles that are absolutely essential for spinal health.
When facet joints get inflamed, they often become stiff or "stuck," which just keeps the pain cycle going. That’s where hands-on therapies, like precise and gentle chiropractic care, come in. The goal is to restore normal motion to these joints, which in turn helps reduce stiffness, improve your ability to move, and dial down the pain signals being sent to your brain.
At Bonesetters, we use the computer-guided PulStar system for our adjustments. This technology allows us to be incredibly precise, applying targeted impulses to restore the joint's natural movement without any of the forceful twisting or cracking you might be picturing.
By addressing the mechanical dysfunction of the facet joints, we can create an environment where the body's natural healing processes can take over more effectively. This is a key step in providing lasting relief.
Combining these foundational therapies often creates a powerful synergy, setting the stage for more advanced non-invasive options that can accelerate healing.
While exercise and manual therapies address the mechanical side of things, advanced technologies can tackle the problem on a cellular level. These treatments are designed to bring down inflammation and speed up tissue repair without any invasive procedures.
Two highly effective technologies we use are:
These technologies are a perfect complement to other conservative treatments. They directly target the biological drivers of pain and inflammation, making them a cornerstone of any modern approach to facet joint care.
To give you a better sense of how these pieces fit together, let's take a quick look at the most common conservative treatments. This table breaks down what each one does and who it's best for.
A quick comparison of common non-invasive treatments, outlining their primary goals, how they work, and who they are best suited for.
| Treatment | Primary Goal | How It Works | Best For |
|---|---|---|---|
| Physical Therapy | Strengthen & Stabilize | Builds core muscle support to unload stressed facet joints. | Patients needing to improve spinal stability and movement patterns. |
| Chiropractic Care | Restore Joint Motion | Uses precise adjustments to improve mobility in stiff or "stuck" joints. | Individuals with mechanical back pain and restricted movement. |
| Laser Therapy | Reduce Inflammation | Delivers light energy to cells to accelerate tissue repair and decrease pain. | Patients with significant inflammation and a need for faster healing. |
| Medications | Manage Symptoms | Temporarily reduces pain and inflammation with NSAIDs or muscle relaxants. | Providing short-term relief to allow for engagement in other therapies. |
Each of these therapies plays a specific role, and they often work best when used together as part of a comprehensive plan.
Finally, never underestimate the power of lifestyle factors. Things like diet can have a huge impact on your body's level of inflammation. Alongside your treatments, learning about inflammation reducing foods can be a simple but powerful way to support your recovery.
By combining activity modification, targeted exercise, precise manual therapies, and advanced non-surgical technologies, we can build a strong and resilient foundation for long-term facet joint pain relief. This multi-faceted approach ensures that we are not just masking symptoms, but addressing the root causes of your discomfort.
So, what happens when conservative treatments just aren't cutting it? If you've done the work with physiotherapy and activity changes but are still struggling, it doesn't mean you've hit a dead end. This is often the point where we look at interventional treatments—more direct, minimally invasive procedures designed to get right to the source of the problem.
The whole idea is to break the cycle of pain. When discomfort is so severe that you can't even participate in your own recovery, these techniques can calm things down enough to give you a fighting chance to heal.

One of the go-to strategies is a therapeutic facet joint injection. It's performed much like the diagnostic blocks we use to confirm where the pain is coming from, but the purpose is entirely different. Instead of just a numbing agent, this injection delivers a small amount of a powerful anti-inflammatory medication (typically a corticosteroid) right into the irritated joint.
Think of it as putting out a fire at its source. By reducing that intense swelling and irritation directly, we can achieve pain relief that often lasts for weeks or even months. For many people, this provides the critical window they need to finally make real progress in physical therapy.
Sometimes, the muscles around the spine also develop painful knots that complicate the picture. In these cases, other techniques like trigger point injections can offer additional relief.
While injections are fantastic for calming flare-ups, they're not always a long-term fix. For more durable results, we often turn to a procedure called radiofrequency ablation (RFA), which you might also hear called a rhizotomy. If your diagnostic medial branch blocks were successful, RFA is the logical next step.
The concept is quite straightforward. We use a specialized needle to deliver a very precise, gentle heat current to the medial branch nerves—these are the tiny nerve fibers that carry pain signals from your facet joint to your brain. This heat creates a small lesion on the nerve, which essentially disrupts its ability to send those pain signals.
RFA doesn’t reverse the arthritis in the joint itself. What it does is “unplug” the pain signal. This can give you a significant period of relief, often 6 to 18 months, to build strength and improve your body mechanics without being limited by constant pain.
It's not a permanent solution because nerves have the ability to grow back over time. However, RFA is a cornerstone of modern pain management, giving people a long-term break from chronic facet joint pain so they can get back to living their lives.
Radiofrequency ablation isn't an experimental procedure; it's a well-established and highly effective tool. We only consider it for patients who have had at least 80% of their pain relief from diagnostic blocks, ensuring we're targeting the right spot.
When that criterion is met, the results speak for themselves. Studies show success rates of around 75% for meaningful pain relief that lasts a full year. By offering this bridge away from chronic pain, interventional treatments empower you to regain control and focus on the ultimate goal: building a stronger, more resilient spine.
While the treatments we've covered are fantastic for managing pain, there's another branch of medicine that asks a bigger question: What if we could help the joint heal itself? This is the core idea behind regenerative medicine, and it marks a real shift in how we think about chronic pain. Instead of just blocking pain signals or tamping down inflammation, these therapies aim to kickstart your body’s own built-in repair crew.
This approach is all about moving beyond managing symptoms and getting to the root of the problem—the damaged tissue. For anyone looking for a lasting treatment for facet joint pain, this is an exciting frontier that focuses on true restoration.
One of the most well-known regenerative options is Platelet-Rich Plasma (PRP) therapy. The logic behind it is beautifully simple. Your blood is filled with platelets, which you can think of as your body's first responders. When you get a cut, they rush to the scene, packed with powerful growth factors that begin the repair process.
PRP therapy simply concentrates these natural healers and delivers them directly to the source of the pain. Here’s how it works:
The goal is to deliver a super-charged army of your body's own repair cells to the arthritic joint. This can help trigger genuine tissue repair, reduce pain, and restore function from the inside out.
This isn't just theory—a growing body of research shows PRP can be highly effective for facet joint pain, especially when you compare it to traditional steroid injections. Steroids are great for providing quick relief by knocking out inflammation, but that relief is often temporary. Regenerative therapies like PRP, on the other hand, aim for a more durable, long-term fix.
Platelet-Rich Plasma (PRP) therapy works by activating the body's innate healing cascade. It's not about masking pain but about creating an environment within the joint that is conducive to cellular repair and regeneration.
A key 2017 study really drove this point home. It found that while both PRP and steroids helped at first, PRP provided much longer-lasting back pain relief. In fact, over 81% of PRP patients still had significant pain relief after six months. For the steroid group, the benefits had mostly worn off after just one month. If you're curious, you can dig deeper into the research on PRP in treating facet-mediated low back pain to see how it stacks up.
This kind of evidence points toward a new way of thinking—one that focuses on true healing. By giving your body the raw materials it needs to mend itself, regenerative medicine offers a path toward not just feeling better, but truly getting better.
When it comes to treating facet joint pain, there’s no single magic bullet. Real, lasting relief comes from a well-thought-out plan that understands your body is an interconnected system. The goal is to build a strategy that’s as unique as your pain, pulling from the different stages of care we've covered.
Your journey has to start with an accurate diagnosis to make sure the facet joints are actually the source of the problem. Once we've confirmed that, we can build a strong foundation with conservative care aimed at getting you moving correctly again. If the pain sticks around, we can then look at more advanced interventions. This step-by-step approach makes sure you get the right care at the right time.
A truly effective plan doesn't just treat the sore joint; it digs deeper to address the reasons it became painful in the first place. This is where an integrated, non-surgical strategy really shines. By combining different therapies, we create a powerful effect where each treatment boosts the effectiveness of the others.
For example, a typical integrated plan might include:
This combination tackles the problem from every angle—mechanical, structural, and biological. You can read more about how our specialists collaborate in our guide on a multidisciplinary approach to pain management.
The goal isn't just to silence symptoms but to create a healthier, more resilient spinal environment. By combining therapies that decompress, realign, and heal, we address the root cause for more durable results.
Living with chronic facet joint pain can feel incredibly limiting, but a clear, evidence-based plan can bring back both hope and function. You shouldn't have to settle for a life defined by discomfort.
The key is to work with a specialist who genuinely listens, performs a thorough diagnosis, and then builds a recovery roadmap specifically for you.
Getting back to a comfortable and active life is absolutely within reach. The first step is a comprehensive consultation to figure out every single factor contributing to your pain. From there, we can build a customized, non-surgical plan to get you back to doing what you love.
When you're dealing with back pain, a lot of questions come up. It's only natural. Below, I’ve answered some of the most common things people ask about facet joint pain to give you a clearer picture of what to expect on the road to recovery.
Everyone wants to know when they'll feel better, and the honest answer is: it depends. The timeline really hinges on the treatment path you take and your body's unique response.
If you’re going the conservative route with physiotherapy or chiropractic care, many people start to feel a difference within a few weeks. But to build real, lasting strength in the muscles that support your spine, you're realistically looking at two to three months of consistent work.
Interventional treatments have their own clock. A therapeutic steroid injection can quiet things down in just a few days, but that relief is often temporary, lasting a few months. For something more durable, radiofrequency ablation (RFA) can be a game-changer. It might take two to three weeks to feel the full benefit, but that relief can last anywhere from six to 18 months. Often, the best results come from a smart combination of approaches that tackle both the immediate inflammation and the underlying joint mechanics.
Yes, it is—and in fact, it’s one of the most important things you can do. The trick is doing the right kind of exercise. High-impact activities or any sudden, forceful twisting of the spine are off the table for now, as they can easily stir up an inflamed joint.
The goal is to focus on low-impact movements that build support without adding stress.
Strengthening these supporting muscles isn't just a treatment—it's your best long-term strategy for keeping facet pain from coming back.
Most of the time, facet joint pain is just that—a painful joint. But there are a few "red flag" symptoms you should never ignore, as they can point to a more serious issue that needs immediate medical evaluation.
It's essential to distinguish between the typical ache of facet syndrome and symptoms that could signal neurological compromise. If you experience any of the following, seek medical help right away.
Keep an eye out for these warning signs:
Preventing a relapse is all about building good habits that create a healthy, resilient spine. Once we get the initial pain under control, the focus shifts from treatment to maintenance.
Here are the most effective strategies for long-term prevention:
Adopting this kind of proactive mindset is what allows you to stay active and in control, significantly reducing the risk of pain returning.
At Bonesetters, we don't believe in one-size-fits-all solutions. We build personalized, evidence-based plans that get to the root cause of your pain. If you're ready to move beyond temporary fixes and create a strategy for lasting relief, we invite you to schedule a comprehensive consultation. Learn how our non-surgical approach can help you reclaim your comfort and mobility.