When pain doesn't just stay in one spot, but instead travels, it's a sign your body is sending a very specific message. This is what we call radiating pain—a sensation that follows the precise path of a nerve.
Imagine a single wire running from a light switch all the way to a bulb. If you pinch that wire near the switch, the light at the other end will flicker or go out. Radiating pain works the same way. The problem might be in your spine (the "switch"), but you feel the strange sensations—the "flickering"—all the way down your arm or leg.
Knowing what to look for is the first step. This isn't your typical dull ache. Because it follows a nerve's specific route, radiating pain has a very distinct and often unsettling character. It's a direct signal that a nerve is being pinched, stretched, or irritated somewhere along its path.
The sensations almost always start from a central point, like your neck or lower back, and then travel outward. Learning to recognize these feelings is key, as the exact path the pain takes gives us vital clues about which nerve is involved and where the trouble is starting.
When people describe radiating pain, a few key descriptions come up time and time again. You might be experiencing it if you feel:
To make it even clearer, here’s a quick breakdown of what to look for.
| Sensation Type | Pain Pathway | Common Descriptors |
|---|---|---|
| Electrical | Travels a long, defined path | "Shooting," "electric shock," "jolt" |
| Thermal | Follows a specific line | "Burning," "searing," "hot" |
| Neuropathic | Occurs along the nerve route | "Tingling," "pins and needles," "numbness" |
| Motor | Affects muscles served by the nerve | "Weakness," "heaviness," "clumsy" |
This table helps summarize the direct link between the sensation and a specific nerve pathway, which is the defining feature of radiating pain.
The real giveaway for radiating pain is its predictability. If pressing on a certain spot in your neck always sends that same jolt down your left arm, that’s a classic sign a nerve root is being squeezed.
A perfect example of this is sciatica, where a sharp pain runs from the low back down the leg. It's caused by irritation of the big sciatic nerve, often from something like a herniated disc. This isn't a minor issue; according to the Global Burden of Disease Study, low back pain—which often includes radiating symptoms—affected a staggering 619 million people globally in 2020. That makes it the single leading cause of disability worldwide.
By recognizing these very specific symptoms, you're not just complaining about pain—you're providing the exact information needed to get to the root of the problem and find lasting relief.
It’s incredibly common to confuse radiating pain with another type known as referred pain. On the surface, they seem similar—both involve feeling pain in one spot when the actual problem is somewhere else entirely. But digging into the why behind each one is the key to a proper diagnosis and, more importantly, effective treatment.
Think of radiating pain like a direct phone line. If a nerve in your spine gets pinched (the source), the signal travels straight down that specific "wire" to its endpoint. This creates a clear, predictable line of pain, tingling, or numbness shooting down your arm or leg.
Referred pain, on the other hand, is more like crossed signals in a busy switchboard. A problem in an internal organ, like your heart, sends out a distress signal. When that signal reaches the spinal cord, it gets jumbled with signals from other parts of the body, like your arm or jaw. Your brain gets confused and misinterprets the source, making you feel pain in your arm when the real issue is your heart.
The biggest giveaway is how the pain travels. Radiating pain is loyal to a single, specific nerve pathway. It’s so predictable, in fact, that we have maps of these pathways called dermatomes. Each dermatome is a patch of skin supplied by a single spinal nerve root.
For example, pressure on the L5 nerve root in your lower back will cause symptoms down a very specific path—the side of your leg, into your big toe. It doesn't just show up randomly. This map-like consistency is a huge clue for doctors.
Referred pain plays by a different set of rules. It’s vague and doesn't follow a clear dermatome pattern. The pain can feel deep, achy, and spread out. The classic example is a gallbladder attack causing pain in the right shoulder—there's no direct nerve line connecting the two, just a shared "circuit" in the spinal cord that scrambles the location data.
The critical takeaway is this: Radiating pain is a direct signal of nerve root irritation that follows a clear, map-like path. Referred pain is a case of mistaken identity, where a problem (often organ-related) causes pain somewhere else due to shared nerve connections.
This illustration shows the direct pathway of radiating pain, starting from the spine and traveling down a nerve.
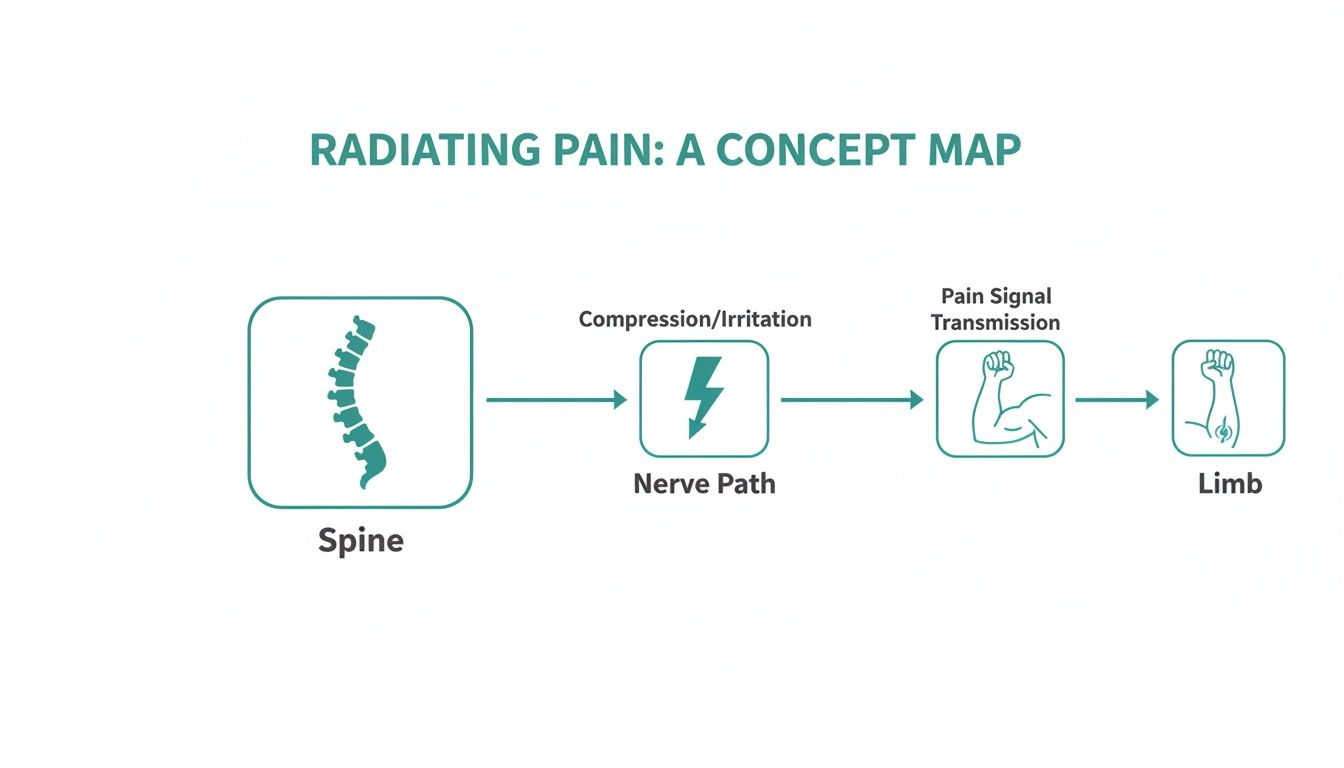
As you can see, the problem originates right at the spinal level and travels along that one nerve, causing symptoms to show up in the arm or leg it controls.
Getting this distinction right is everything. If your pain is radiating, the treatment has to target the source of the nerve compression in your spine. That’s where therapies like spinal decompression come in—they work to take the pressure off that specific nerve root.
But if the pain is referred, treating the spine would be a complete waste of time. The focus would need to shift to the actual source, whether it's an internal organ or a deep muscular trigger point. This is why it’s so vital for you to tell your doctor exactly where your pain starts, the path it travels, and what it feels like. You’re essentially giving them the roadmap to a successful diagnosis.
To really get to the bottom of radiating pain, we have to look past the symptoms and find the source. That shooting, burning, or tingling feeling is just an alarm bell; the real question is, what's tripping the wire? In almost every case, the culprit is a mechanical issue or health condition that's physically irritating a nerve and scrambling its signals.
Think of a garden hose hooked up to a spigot. If you step on the hose right where it connects to the faucet, the water flow to the sprinkler at the other end sputters and weakens. That's a perfect way to visualize the most common cause of radiating pain.

The problem isn't the sprinkler—it's the pinch point at the source. Any effective treatment has to focus on taking that pressure off, not just fiddling with the sprinkler.
The official term for this "pinched hose" problem is radiculopathy. It happens when a nerve root—the very beginning of a nerve as it branches off the spinal cord—gets compressed or inflamed. This is the main reason people experience radiating pain that starts in their neck or lower back.
When that pressure hits, it disrupts the nerve’s ability to work properly, causing it to misfire and send those faulty signals of pain, numbness, or weakness down its entire path.
Several common spinal problems can lead to radiculopathy, each putting the squeeze on a nerve root in its own way.
The most famous example of radiculopathy? Sciatica. It’s not a diagnosis on its own but a description of symptoms that arise when the sciatic nerve roots in the low back are compressed. The result is that all-too-familiar pain that travels down the back of the leg, sometimes reaching all the way to the foot.
While radiculopathy is a problem at the nerve’s starting point, another major cause of radiating-style pain involves damage happening further down the line. This is called peripheral neuropathy. Instead of a single pinch point at the spine, think of this more like the electrical wiring itself becoming frayed and damaged throughout the system.
Peripheral neuropathy is often the result of systemic health problems that affect the entire body, leading to widespread nerve damage.
Unlike the localized compression of radiculopathy, peripheral neuropathy typically causes symptoms that are more symmetrical, often affecting both hands or both feet in a "glove and stocking" pattern.
Common culprits behind this condition include:
Figuring out these distinctions is everything. Is your pain coming from a single, mechanical pinch point in your spine, or is it a sign of a larger, body-wide issue affecting your nerves? The answer completely changes the treatment plan, which is why getting an accurate diagnosis is the most critical first step toward relief. The scale of these issues is enormous; globally, low back pain—a primary driver of radiating pain—affected an estimated 628.8 million people in 2021 alone. You can learn more about the global impact of low back pain in this detailed public health report.
Your body has a way of telling you when something is wrong, and pain is one of its loudest signals. With radiating pain, these signals tell a very specific story—one about a nerve that’s being squeezed, stretched, or irritated. Learning to read these signs is key to knowing when you should book a specialist appointment versus when you need to head to the emergency room.

The feeling of radiating pain is different for everyone, but it’s rarely just a simple ache. Because it’s coming directly from an agitated nerve, the symptoms have a distinct neurological flavor.
If you're experiencing any of the feelings below, it's a good bet that a nerve is in trouble. Think of these as your body’s early warning system, signaling that it’s time to see a specialist to figure out what's really going on before it gets worse.
Common signs include:
These symptoms are your cue to take action. While they are certainly serious, there's another level of symptoms that demand a much faster response.
While the symptoms above are important, some signs point to severe nerve compression that could cause permanent damage if not treated immediately. These are true medical emergencies.
If you experience any of the following "red flag" symptoms, don't wait to schedule an appointment. Go to an urgent care center or an emergency room right away.
These critical warnings can indicate a serious condition like cauda equina syndrome or severe spinal cord compression, where the bundle of nerves at the base of your spine is being dangerously squeezed.
Seek emergency care if you experience:
This table is a quick reference to help you tell the difference between symptoms that need a specialist's attention and those that require a trip to the ER.
| Symptom Category | Common Manifestation (Consult a Specialist) | Red Flag Warning (Seek Immediate Medical Care) |
|---|---|---|
| Sensation | Tingling, "pins and needles," or localized numbness. | Complete numbness in the groin or "saddle" region. |
| Motor Control | Mild muscle weakness, like a weak grip or a heavy leg. | Progressive weakness making it hard to walk; "foot drop." |
| Bowel/Bladder | Normal function. | Sudden and new loss of bowel or bladder control. |
Understanding this distinction is crucial. Most cases of radiating pain can be managed effectively with the right non-surgical care, but ignoring red flags can have life-altering consequences. Learning to spot these urgent signals empowers you to make smarter, safer decisions and get the right care when you need it most.
Figuring out the true source of radiating pain is a bit like being a detective. We can't just chase the symptoms; we have to follow the clues back to the scene of the crime. The entire process is methodical, starting with the single most important tool we have: a simple, thorough conversation with you.
Your story gives us the first clues. When did the pain start? What does it really feel like—is it sharp, dull, burning, or tingling? What makes it better or worse? These details are invaluable. Right after our talk, we move on to a hands-on physical exam, which is where we start to physically map out the nerve pathway that's causing all the trouble.
The physical exam isn’t just a random set of movements. It’s a targeted series of orthopedic and neurological tests, each one designed to provoke your specific symptoms and pinpoint the exact nerve root that's irritated.
We’ll typically run through a few key tests:
The whole point of these hands-on tests is to isolate the problem. By systematically confirming some nerve paths and ruling out others, we can zero in on the exact spot in your spine where the irritation is happening.
Most of the time, a thorough physical exam gives us a very clear picture. But sometimes, we need to see exactly what’s going on under the surface to confirm our findings. That’s where advanced imaging like a Magnetic Resonance Imaging (MRI) scan comes in. An MRI is rarely the first step; it's a powerful tool we use to verify what the exam already strongly suggests.
An MRI gives us an incredibly detailed look at your soft tissues—the spinal discs, ligaments, and the nerves themselves. It can show, without a doubt, a herniated disc pressing on a nerve or the bony overgrowth from spinal stenosis that's crowding the nerve canal. Seeing this confirmation is what allows us to build a truly precise treatment plan.
If you’re interested in the diagnostic process, you can learn more about how chiropractors know where to adjust in our detailed guide.
By putting together your story, the findings from a detailed exam, and, when needed, targeted imaging, we create a complete picture of your radiating pain. This evidence-based approach takes the guesswork out of the equation and lets us get straight to a focused, effective plan to get you feeling better.
Once we’ve pinpointed exactly where that radiating pain is coming from, the entire game plan shifts to fixing the underlying problem. Instead of just chasing the pain with medication, modern non-surgical treatments are all about tackling the root mechanical issue—the thing that’s actually squeezing the nerve. The goal isn't a temporary fix; it's a lasting solution that helps your body heal itself.
This means we go after the herniated disc, bone spur, or narrowed spinal canal that’s pinching the nerve. By taking the pressure off, we can finally stop those pain signals at their source.
One of the most powerful ways to relieve nerve pressure is with Chiropractic Decompression. Remember that garden hose analogy? Imagine a heavy rock sitting on it, stopping the water flow. Decompression therapy is like gently and carefully lifting that rock off the hose, letting the water rush through again.
This treatment uses a highly specialized table that applies a slow, controlled stretch to the spine. This gentle pull creates a negative pressure inside the disc, which can help draw the bulging or herniated material back into place and away from the nerve. It literally creates more space for the nerve to exist without being choked off.
Creating space is step one. Step two is getting the joints moving correctly again. To do this, modern chiropractic care often uses incredible tools like the PulStar system, a computer-guided instrument that delivers incredibly precise and gentle adjustments.
This technology analyzes the motion of each spinal joint and sends targeted impulses only to the areas that are stuck. It restores normal movement without any of the forceful twisting or cracking some people associate with older techniques. It's a comfortable, objective way to improve how your spine functions, which is essential for any real, long-term healing.
The combination of creating space with decompression and restoring motion with precise adjustments is a powerful one-two punch. It tackles the mechanical causes of radiating pain from multiple angles, giving your body the support it needs to heal properly.
The need for effective, non-invasive solutions like these is only growing. Radiating pain from low back issues is now the leading cause of years lived with disability globally, a trend that started back in 1990. Shockingly, projections estimate that the number of cases will climb to 843 million, with women and older adults being disproportionately affected.
Beyond the mechanical fixes, we can also accelerate healing deep within your cells. Class IV Cold Laser Therapy, for example, uses specific wavelengths of light that penetrate deep into damaged tissue.
This light energy stimulates the mitochondria—the powerhouses of your cells—ramping up energy production. This, in turn, reduces inflammation, improves local circulation, and speeds up the repair of damaged tissue. It’s a way to calm the irritated nerve itself and heal the surrounding tissues that have taken a beating.
A comprehensive approach often brings in other key elements:
For many people, specialized rehab like in-home physical therapy becomes a critical part of recovery, especially when mobility is a challenge. By layering these modern, evidence-based treatments, we can create a clear path toward lasting relief from radiating pain. Our guide on the best treatments for nerve pain explores these options even further.
When you're dealing with pain that travels, a lot of questions can pop into your head. It's completely normal to feel uncertain. Let's walk through some of the most common concerns we hear from patients to give you the clarity you need to move forward.
It's a tempting thought—maybe if you just ignore it, it'll disappear. While some minor aches might fade, radiating pain is different. It’s a direct signal from an irritated nerve, often caused by a mechanical issue like a herniated disc or spinal stenosis. Left alone, the underlying problem can actually get worse.
Think of it like your car's "check engine" light. It’s pointing to a specific issue that needs attention. Ignoring the warning light doesn’t fix the engine, and ignoring radiating pain won’t fix the nerve compression. Addressing the root cause is the only way to prevent chronic pain, further irritation, and potentially lasting damage.
Not always, but it's always a sign that a nerve is unhappy. Radiating pain is your body's way of telling you that something is pressing on or inflaming a nerve, and that’s a message you should listen to. The good news? The majority of causes are very manageable with the right non-surgical care.
The key is learning to tell the difference between typical symptoms and true "red flags." As we discussed earlier, things like a sudden loss of bowel or bladder control are medical emergencies. For most other cases, a proper diagnosis is the first step toward a safe and effective treatment plan.
The vast majority of radiating pain cases are resolved successfully with non-surgical treatments like spinal decompression and targeted adjustments. Our goal is always to help you heal and avoid invasive procedures whenever possible.
Everyone's timeline is a little different because it really depends on the specific cause and how long you've been dealing with it. Some people feel a significant improvement after just a few sessions. For others, especially those with more chronic conditions, it might take a bit longer to get lasting relief.
Our approach is to create a personalized plan that gets to the root of the problem, not just chase the symptoms. We focus on providing immediate relief while also building long-term stability so the issue doesn't come back. It's all about making steady, measurable progress and getting you back to your life.
This is probably the biggest fear people have, but let me put your mind at ease: surgery is rarely the first step. For the overwhelming majority of people with radiating pain, conservative, non-invasive treatments are incredibly effective.
Surgery is typically a last resort, reserved for the most severe cases or when those urgent red flag symptoms appear. The primary goal is always to fix the mechanical problem without an operation, allowing your body to heal naturally and helping you sidestep the risks and long recovery that come with surgery.
At Bonesetters Critical Chiropractic, we specialize in finding the true source of your radiating pain and creating evidence-based, non-surgical plans to help you reclaim your life. If you're ready to stop hurting and start healing, schedule your consultation today.