Yes, you can absolutely find lasting relief from a bulging disc without surgery. The secret isn't a quick fix or a miracle cure. It’s a dedicated, phased approach that starts with immediate pain relief and builds toward long-term spinal health.
If you're dealing with the pain of a bulging disc, the thought of surgery can be overwhelming. The good news? The vast majority of people—upwards of 90%—get better with conservative, non-surgical care.
The entire philosophy is different from a surgical one. Instead of just cutting out the problem tissue, we focus on creating the ideal environment for your body to heal itself. We then build up the strength and stability around your spine to make sure this doesn't happen again. This isn't a passive "wait and see" game; it's an active recovery process.
A successful non-surgical plan isn't just one magic bullet. It’s a journey that moves you from being stuck in acute pain to feeling strong, mobile, and confident in your back again. It's a smart combination of what you do at home, what we do in the clinic, and small but powerful lifestyle changes.
I find it helps to break the journey down into three clear phases:
The Relief Phase: Right now, the top priority is to get you out of pain. We need to calm the inflammation and take the pressure off that pinched nerve. This means gentle movements, smart rest strategies, and professional therapies designed for immediate relief.
The Healing Phase: Once the initial crisis is under control, we shift focus to true tissue repair. This is where targeted exercises and more advanced therapies like spinal decompression can make a huge difference. They work to gently retract the bulging disc and boost healing circulation. If you're curious about how that works, you can find a ton of information in these spinal decompression therapy reviews.
The Strength Phase: This is where you build a bulletproof back. The final stage is all about creating a strong, stable core and teaching your muscles how to support your spine correctly during daily activities. This is what dramatically lowers your risk of this ever happening again.
The goal of non-surgical care isn't just a temporary patch-up. It's about restoring full function, fixing the root mechanical issues, and giving you the knowledge and tools to keep your spine healthy for the long haul.
To give you a clearer picture, this table breaks down what to expect during each stage of your recovery.
| Recovery Phase | Primary Goal | Key Actions and Therapies | Typical Duration |
|---|---|---|---|
| The Relief Phase | Reduce acute pain, inflammation, and nerve compression. | Rest, ice/heat, anti-inflammatory nutrition, gentle mobility (e.g., McKenzie exercises), chiropractic adjustments, gentle decompression. | 1 to 4 weeks |
| The Healing Phase | Promote tissue repair, improve disc hydration, and restore normal movement. | Progressive therapeutic exercises, spinal decompression therapy, Class IV laser, core activation, ergonomic adjustments. | 4 to 12 weeks |
| The Strength Phase | Build core and spinal stability to prevent re-injury. | Advanced core strengthening (planks, bird-dog), functional movement training, strength training with proper form, lifestyle integration. | 3 to 6+ months |
This phased approach ensures we're always doing the right thing at the right time—never pushing too hard too soon, but consistently making progress.
This visual timeline gives a great overview of how you'll progress from that initial flare-up to building a back that can support you for life.
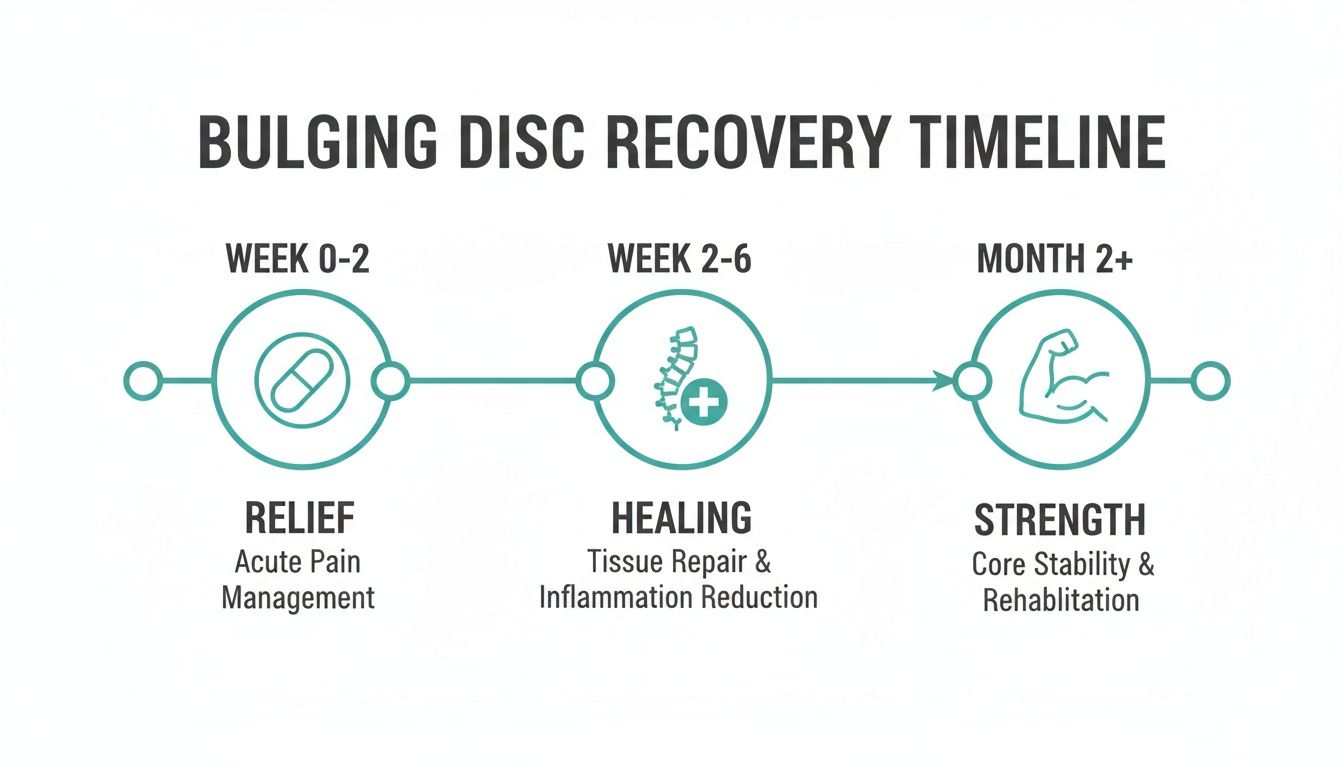
As the graphic shows, recovery is a process. It starts with getting the symptoms under control, but the real work—and the lasting results—come from progressing toward a strong, resilient spine.
When a bulging disc decides to flare up, those first 24 to 72 hours are a battlefield. The pain can be sharp, unrelenting, and frankly, a bit scary. Your first mission isn't to "fix" the disc right away. It's about crisis management—calming the intense inflammation, easing the muscle spasms that lock up your back, and soothing the irritated nerve. Getting this right from the start sets the stage for a much smoother recovery.

The cornerstone of any effective bulging disc treatment without surgery begins with tackling that initial firestorm of inflammation. This is where knowing how to use ice and heat properly makes all the difference.
It’s almost a reflex to grab a heating pad for back pain, but during an acute flare-up, that can be like pouring gasoline on a fire. Heat brings more blood flow, which sounds good but can actually ramp up the inflammation in the first couple of days.
Key Takeaway: It's a simple but powerful rule: ice for inflammation, heat for muscle tension. Use them in that order, and you’ve got a fantastic home-based strategy for pain control.
When the pain is at its peak, even just lying down can feel impossible. The goal is to find a position that takes the pressure off your spine and the angry nerve. Lying flat on your back or stomach can often make things worse by increasing the load on your discs.
Instead, try one of these positions that we recommend to patients all the time:
And please, try to avoid sinking into a soft, deep couch. It forces your spine into a "C" shape that puts maximum pressure on your discs. If you have to sit, place a small rolled-up towel in the curve of your lower back to maintain its natural arch.
I know it feels like the last thing you should do, but strict bed rest is an outdated approach that can actually slow down your recovery. Staying completely still for days on end causes the supporting muscles to weaken and the joints to stiffen, making it much harder to get moving again.
The key is gentle, pain-free motion.
A pelvic tilt is the perfect place to start. While lying on your back with your knees bent and feet flat, gently press the small of your back into the floor by tightening your abdominal muscles. You’re not lifting your hips, just subtly rocking your pelvis. Hold for a couple of seconds, then release. This tiny movement wakes up your core muscles and keeps your spine from seizing up, all without putting any strain on the disc itself.
Once you’ve managed to calm down the initial, intense pain of a bulging disc, the game plan shifts. We move from crisis management to constructive healing, and this is where strategic exercise becomes your most powerful ally.
This isn't about grinding through painful workouts. It's about methodically building a natural "corset" of muscle around your spine to protect the healing disc. Think of it as creating an internal support system. This is a non-negotiable part of any effective bulging disc treatment without surgery.

The goal here is a safe progression, moving from gentle activation to functional strength. Every movement should support your recovery, not cause a setback. We start with the absolute basics: waking up the deep stabilizing muscles that have likely gone dormant.
Before you can strengthen, you have to activate. I'm talking about the deepest core muscles, like the transverse abdominis and multifidus. These muscles act like a built-in weight belt, creating internal pressure that stabilizes your spine from the inside out. After a disc injury, these muscles often "switch off."
Your first mission, then, is to simply switch them back on without aggravating your back. The bird-dog exercise is perfect for this.
The secret is control, not height. Lifting your arm or leg too high forces your low back to arch, which completely defeats the purpose. This slow, deliberate movement re-trains your brain and muscles to work together again, building that crucial stable base.
With a stable foundation established, you can introduce gentle movements designed to encourage the bulging disc material to retract toward the center of the disc. This phenomenon, known as centralization, is a cornerstone of the McKenzie Method.
The goal is to move the pain out of your leg or buttock and back to the center of your lower back. This is a very good sign, indicating the nerve is being decompressed. The classic exercise for this is the McKenzie press-up (or prone press-up).
This extension movement can create a subtle pressure change that helps draw the bulge away from the spinal nerves. If this movement causes your pain to worsen or travel further down your leg, stop immediately and consult a professional.
A patient I once worked with, Sarah, had sciatic pain all the way down to her calf. After a week of consistently doing gentle press-ups, she reported the calf pain was gone, and she only felt a dull ache in her low back. This was a huge win—it was classic centralization in action, showing us the nerve was healing.
Once your core is firing properly and your pain has begun to centralize, it’s time to strengthen the larger muscles that support your entire spinal and pelvic structure. Your glutes are especially important here. From years of clinical experience, I can tell you that weak glutes almost always lead to an over-stressed lower back.
The glute bridge is a fantastic and safe way to build this support system.
This simple movement strengthens the glutes and hamstrings, which act as a powerful support sling for your lower back, taking a massive amount of daily strain off your discs.
If you’re looking for a wider variety of movements, our guide on the best exercises for lower back pain relief offers several other safe and effective options. Just remember, consistency trumps intensity every time. Performing these foundational exercises correctly and regularly is the secret to building a resilient spine and achieving lasting healing without surgery.
While your efforts at home with exercise and self-care are absolutely the foundation of recovery, bringing in professional conservative therapies is how we truly accelerate and solidify the healing process. These treatments aren't just about managing pain; they're designed to target the root biomechanical and physiological problems causing your disc to bulge in the first place.
Think of it like this: your home care is the essential, regular maintenance for your car. But when something is mechanically wrong with the engine, you need a specialist with the right tools. That's where we come in. By combining advanced technology with years of clinical experience, we can create the ideal environment for your disc to heal faster, more completely, and with a much lower chance of future flare-ups.
This is the cornerstone of modern, non-surgical disc treatment, and for good reason. Non-Surgical Spinal Decompression is a highly sophisticated, computer-controlled therapy that gently relieves pressure on your spinal discs and nerves.
It’s far more advanced than simple traction, which often causes your muscles to tense up and resist the pull. Decompression therapy uses a precise, logarithmic pull-and-release pattern that outsmarts the body's natural tendency to guard, allowing the spine to decompress safely and effectively.
It's a bit like pulling apart a compressed sponge so it can soak up water again. Decompression works in a similar way:
The clinical results for spinal decompression speak for themselves. Success rates consistently fall between 71% and 89% across multiple studies. One landmark 2012 study showed that 86% of patients who were already scheduled for back surgery were able to cancel their procedures after completing a decompression protocol. The same study reported a 76.4% overall success rate and an average disc height gain of 1.3 millimeters, proving it can physically restore spinal structure. You can read more about these impressive spinal decompression success rates.
The words "chiropractic adjustment" can sometimes bring to mind forceful twisting or cracking. I want to be clear: modern, evidence-based care has evolved far beyond that. In our office, we use the PulStar system, an FDA-cleared technology that delivers incredibly precise and gentle adjustments without any popping or twisting.
The PulStar uses a handheld instrument to analyze the motion of each individual joint in your spine. It pinpoints exactly which areas are "stuck" or not moving correctly—the very dysfunctions that put extra stress on your discs. The system then delivers a series of light, targeted impulses to restore normal motion only to those restricted joints.
This approach is remarkably specific and comfortable, making it a safe and powerful part of bulging disc treatment without surgery. It's especially valuable for patients who are in acute pain or understandably nervous about traditional manual manipulation. If you're curious, you can learn more about how do chiropractic adjustments work and the science behind these advanced techniques.
We’re not just moving bones around; we’re restoring neurological function. When a joint is moving properly, it sends the right signals to the brain, which helps reduce pain perception and allows the surrounding muscles to relax. It’s about re-establishing communication within the nervous system.
While decompression and adjustments fix the mechanical problems, other therapies we use work at a cellular level to supercharge tissue repair and put out the inflammatory fire.
This isn't science fiction; it's a powerful therapeutic tool grounded in real science. The Class IV Cold Laser uses specific wavelengths of light that penetrate deep into the damaged tissue surrounding your disc. This light energy is absorbed by your cells' mitochondria—their powerhouses—and kicks off a process called photobiomodulation.
This process does a few critical things:
Another powerhouse modality we use is Horizontal Stimulation Therapy. This is a highly advanced form of electrical stimulation that is far more comfortable and effective than a typical TENS unit you might buy at a store.
Instead of just buzzing the surface, it creates a bioelectric field at the cellular level. This helps to block pain signals before they reach the brain while also reducing swelling and deep muscle spasms. It is incredibly effective at calming the severe nerve irritation—sciatica or radiculopathy—that so often comes with a bulging disc.
When used together, this combination of therapies creates a synergistic healing effect. We are decompressing the disc, restoring proper joint mechanics, and fueling the body's own repair processes all at the same time. This integrated strategy is why we see faster, more durable results than with any single therapy alone. It’s the professional difference that helps you not just feel better, but truly get better.
Let's be honest: effective, long-term relief from a bulging disc goes way beyond what happens in a clinic or during your exercises. The real magic, the stuff that makes the healing stick, is built on the small, consistent choices you make every single day. You have to create an environment where your body can actually heal, 24/7.

This is about getting serious about what you eat, how you sit, and the way you sleep. These daily habits can either be powerful allies in your recovery or they can quietly sabotage your progress by fueling inflammation and putting constant, low-level stress on your healing spine.
Inflammation is a huge part of the pain equation with disc injuries. While in-office therapies like laser treatment are fantastic for targeting it locally, the food you put in your mouth has a massive impact on your body’s overall inflammatory state.
Think of your food as a tool. The right foods can actively calm inflammation and provide the essential building blocks your body is crying out for to repair that damaged disc.
Foods to Load Up On:
On the flip side, some foods can be like pouring gasoline on a fire, promoting a state of chronic, low-grade inflammation that works directly against your recovery.
Foods to Minimize or Avoid:
My go-to advice for patients is simple: focus on whole, unprocessed foods. If it grew in the ground, on a plant, or had a healthy life, it's probably going to help your spine heal.
You could be doing everything right in your treatment plan, but if you spend eight hours a day slouching in a chair that constantly compresses your disc, you're taking one step forward and two steps back. Small, mindful adjustments to your environment can take a surprising amount of daily strain off your lower back.
At Your Desk:
In Your Car:
Sleep isn't just rest; it's prime time for repair. This is when your body gets down to business, releasing growth hormone and other compounds essential for healing damaged tissues, including the cells in your discs.
But your sleeping position can make or break this process. Stomach sleeping is the absolute worst for a disc injury—it forces your lower back into an exaggerated arch and twists your neck for hours.
Spine-Safe Sleeping Positions:
These lifestyle changes are so powerful because their effects are cumulative. Each smart choice builds on the last, supporting your body's incredible ability to heal itself. We see this validated in research, too. Conservative plans that combine professional care with these exact lifestyle changes get amazing results. Studies have shown disc reabsorption rates (where the body literally heals the bulge) as high as 77.9% with this approach.
In one compelling study, 112 out of 136 patients showed measurable disc regression on their MRIs after just 6-12 sessions of targeted therapy and lifestyle coaching. If you want to dig into the data, you can read the full study about these conservative treatment outcomes. It’s powerful proof that what you do every day is just as important as the treatment you receive.
Look, the overwhelming majority of bulging discs get better without surgery. That’s the whole point of this guide. But part of a smart, conservative treatment plan is knowing when it's time to call in the cavalry.
Your body has a way of telling you when a problem is bigger than you can handle at home. We call these "red flags"—symptoms that could point to serious nerve compression. Ignoring them is a bad idea, as it could lead to permanent damage.
If you experience any of the following, don't delay. This isn't about being tough; it's about being smart. These signs can indicate a rare but serious condition called cauda equina syndrome, which is a true medical emergency.
These symptoms require an immediate medical evaluation.
So, what happens if there are no red flags, but you've been doing everything right for weeks and you're still not getting better? This is when a surgical consultation might come up.
It's important to go into that conversation with your eyes wide open. Surgery can be the right answer for some people, but it’s not a magic bullet.
Let's look at the evidence. A huge meta-analysis that reviewed outcomes for over 39,000 lumbar disc surgery patients found that only 78.9% had good or excellent long-term results.
You can dive into the details yourself by checking out the study on the long-term outcomes of lumbar disc surgery.
The takeaway here isn't that surgery is bad. It's that surgery isn't a guaranteed fix. This is exactly why we emphasize exhausting all the powerful, effective conservative options first. They work for most people, and they carry far fewer risks.
Deciding to tackle a disc injury without surgery brings up a lot of questions. That’s completely normal. Getting clear, honest answers is the first step toward feeling confident in your recovery plan. Let's walk through some of the things our patients ask us every day.
Everyone’s body is a little different, but most people start to feel a real, tangible improvement within the first couple of weeks of consistent care. A full, non-surgical treatment plan for a bulging disc typically takes about 6 to 12 weeks.
That timeframe gives us enough runway to not just get you out of that initial, acute pain, but to also move you through the critical phases of healing and strengthening. The immediate goal is relief, but the long-term win is building a stronger, more resilient back to keep this from happening again.
While our bodies are incredible healers, a significant disc bulge rarely gets back to 100% without some help. If you don't actively work to decompress the spine and fix the underlying movement problems that caused the bulge in the first place, that disc often becomes a permanent weak link.
Simply resting and waiting it out can be a recipe for chronic pain, lingering muscle weakness, and a much higher chance of re-injuring yourself down the line. A proactive treatment plan doesn't just wait for healing—it guides it, leading to a much more complete and lasting recovery.
Yes, absolutely—as long as it’s the right kind of chiropractic care. Forget the old stereotype of aggressive twisting and popping. Modern, evidence-based chiropractors use gentle, precise techniques that are specifically designed for fragile disc injuries.
Here in our clinic, we rely on methods like:
These advanced, low-force approaches are what make chiropractic such a safe and effective cornerstone of non-invasive disc recovery.
It helps to think of your spinal disc as a jelly donut.
A bulging disc is like squishing the whole donut. The outer wall swells and bulges outward pretty evenly, but the jelly on the inside (the nucleus) is still contained.
A herniated disc happens when a tear or crack develops in that outer wall, letting some of the jelly leak out. It’s generally a more significant injury.
The key takeaway, however, is that both conditions cause pain by putting pressure on nearby nerves. And importantly, both respond incredibly well to the conservative, non-surgical treatments we've been discussing. The mission is always the same: get the pressure off the nerve and create the right environment for the body to heal.
At Bonesetters Critical Chiropractic, we specialize in guiding patients through this exact recovery process. If you're ready to find lasting relief without surgery, explore our evidence-based approach at https://bonesetters.org.