When you're trying to figure out the best way to treat knee arthritis, it’s not about finding a single magic bullet. It’s about building a personalized strategy that works for you. The right approach really depends on the stage of your arthritis, your lifestyle, and what you want to achieve, often by combining a few different methods to manage pain and get you moving again.
Living with knee osteoarthritis can feel overwhelming, but getting a clear picture of your options is the first real step toward taking back control. While there's no universal cure, a well-structured treatment plan can make a world of difference in your mobility and pain levels. The journey almost always starts with the basics—foundational, non-invasive strategies—and only moves on to other options when necessary.
This guide breaks down the four main categories of treatment, comparing them side-by-side. We’ll look at how each one fits into a complete care plan, so you can walk into your doctor's office ready to have a more informed conversation. The goal is to give you the knowledge you need to manage your symptoms and, most importantly, improve your quality of life.
Managing knee arthritis effectively usually means layering different approaches. The primary treatment paths fall into four main categories:
Leading international guidelines all agree: start with conservative care first. For example, research has consistently shown that a 5–10% reduction in body weight can bring about a major drop in pain and disability for those who are overweight, sometimes even delaying or preventing the need for surgery down the road. You can find more details in these important knee pain statistics.
Navigating your treatment path requires a clear understanding of what each option offers. The most successful outcomes always come from a partnership between an informed patient and a knowledgeable healthcare provider.
To help you see how these categories fit together, here's a quick overview of their primary goals and who they're best suited for.
| Treatment Category | Primary Goal | Best For |
|---|---|---|
| Conservative Care | Reduce joint stress and inflammation naturally | Early-stage arthritis; all patients as a foundational strategy. |
| Physical Therapies | Improve strength, stability, and function | Patients with muscle weakness or poor biomechanics. |
| Injections | Provide targeted, temporary pain relief | Moderate to severe pain flare-ups; delaying surgery. |
| Surgery | Permanently resolve pain and restore function | End-stage arthritis when other treatments have failed. |
Think of these categories as a roadmap. Most people start at the top and only move down the list if their symptoms aren't improving enough, always with the guidance of a trusted healthcare professional.

When you're trying to figure out the best treatment for knee arthritis, the first stop is almost always the foundational, non-invasive strategies. This is where we talk about conservative management and structured physical therapies—the bedrock of any smart plan. They both have the same goal: get you moving better with less pain, no surgery required. But they aren't the same thing. The real difference comes down to structure, intensity, and who's guiding the process.
Think of conservative management as the lifestyle changes you can start today. This is all about low-impact exercises like swimming or cycling, cleaning up your diet to fight inflammation, and getting to a healthy weight to take some stress off those knees. The big plus here is that you're in the driver's seat.
Structured physical therapy, on the other hand, is a personalized program run by a licensed pro. It’s not just "exercise." It’s a specific prescription of movements, stretches, and other treatments built to fix your unique biomechanics, weak spots, and functional hurdles.
One of the most important distinctions to understand is the difference in commitment and how long it takes to see results. Self-directed conservative care takes a ton of personal discipline and consistency. You're playing the long game here. The improvements are slow and steady over months, but the payoff is a sustainable, healthier life overall.
With physical therapy, you'll often feel a difference much faster, sometimes in just a few weeks. Having a therapist keeps you accountable and makes sure you're progressing your exercises correctly and safely. That expert guidance can be a game-changer, especially when pain makes it tough to even think about starting on your own.
Key Insight: Conservative management is a marathon focused on building sustainable lifestyle habits. Structured physical therapy is more like a targeted boot camp, designed to build strength, fix your form, and accelerate your progress in a shorter, more intense window.
So, which one is the right place for you to start? Let’s break it down side-by-side.
| Feature | Self-Directed Conservative Management | Structured Physical Therapy |
|---|---|---|
| Guidance | You're in charge, relying on general health principles. | Professionally guided by a licensed physical therapist. |
| Focus | Overall wellness, weight management, and gentle activity. | Fixing specific muscle imbalances, stability, and biomechanics. |
| Timeline | Gradual improvements over several months. | Faster, more noticeable gains in 4-12 weeks. |
| Ideal For | Early-stage arthritis or as a foundational habit for everyone. | Moderate arthritis, post-injury recovery, or poor movement patterns. |
If you have mild, early-stage knee arthritis, diving into conservative management is the perfect first step. Things like daily walks and adopting an anti-inflammatory diet are great habits that reduce joint load and keep symptoms from getting worse. This approach truly empowers you to manage your own health.
But what if your pain is more significant? Or you feel unsteady? Or you just have no idea which exercises are safe? That’s your cue to start with a physical therapist. A good PT can spot underlying issues—like weak hips or quads that are secretly stressing your knee—and give you targeted exercises to fix them. They’ll also drill you on proper form, which is critical to avoid making things worse.
Many physical therapists also have other tools in their toolkit to speed up recovery and knock down pain. They might use manual therapy (hands-on joint work), heat and cold therapy, or electrical stimulation. Some clinics even offer advanced treatments like therapeutic ultrasound to manage deep-tissue inflammation. You can learn more about what is therapeutic ultrasound and see how it might fit into a comprehensive plan.
In the end, this isn't an "either/or" choice. These two approaches are partners. Physical therapy gives you that initial boost, education, and targeted strengthening. Then, the conservative lifestyle habits you build ensure you protect those gains for the long haul. It's that powerful one-two punch that gives you the best shot at managing your arthritis for years to come.

When the foundational work of exercise and physical therapy isn’t cutting it during a painful flare-up, injections can bring powerful, targeted relief right where you need it—inside the knee joint. They represent a common next step, offering a way to calm things down and get you moving again without the major commitment of surgery.
But here’s the thing: not all knee injections are the same. The three main players—Corticosteroids, Hyaluronic Acid (HA), and Platelet-Rich Plasma (PRP)—each work in a completely different way. Getting to know how they differ in their mechanism, speed, and staying power is the key to picking the right one for your knee.
Think of corticosteroids as the fire extinguisher for an angry, inflamed knee. These are powerful anti-inflammatory drugs injected directly into the joint to shut down the processes causing all that pain and swelling.
This makes steroid shots a fantastic tool for acute flare-ups. Let's say you have a wedding or a big trip planned, but your knee suddenly blows up and is excruciating. A corticosteroid shot can deliver significant relief fast, often within 24 to 72 hours, letting you get back to your life.
The catch? This speed comes at a price. The relief is all about pain control, not healing, and it’s temporary. The research is clear: while the initial relief is great, it tends to peak in the first few weeks and often starts to fade after a month or two.
Hyaluronic Acid (HA) injections, often called “gel shots,” are a different beast entirely. Your joints naturally contain HA in the synovial fluid that lubricates and cushions them. In an arthritic knee, that fluid thins out. HA injections are designed to supplement it.
The goal here isn't a quick fix for sharp pain. Instead, HA works to restore some of that cushioning, which can improve how the joint moves and gradually reduce pain over a longer haul. Most people feel the best results several weeks after they’ve finished their series of injections.
This makes HA a much better fit for someone dealing with chronic, moderate arthritis—that constant, nagging ache and stiffness that makes walking or climbing stairs a daily grind.
Intra-articular corticosteroid injections typically provide short-term pain relief peaking around 1–4 weeks and waning by 12 weeks in many trials. In contrast, intra-articular hyaluronic acid (IA-HA) shows modest benefits that often peak at 8 weeks and may persist up to 24 weeks in some studies. As you can learn more in this comprehensive analysis, guideline recommendations vary because the clinical improvements are often considered small to modest.
Platelet-Rich Plasma (PRP) is a more modern, biological strategy. The process uses your own blood, which is drawn and spun down in a centrifuge to isolate and concentrate the platelets. This golden, platelet-rich liquid is then injected back into your knee, full of natural growth factors.
The theory behind PRP is that these growth factors can kickstart your body’s own healing and repair mechanisms. The aim is to do more than just mask symptoms—it’s about reducing inflammation, potentially slowing cartilage breakdown, and improving the overall health of the joint.
Because it relies on triggering a biological response, the relief from PRP comes on slowly. It can take several weeks or even a few months to notice a real difference. PRP is often a consideration for active people with mild to moderate arthritis who want to try an option that addresses the underlying biology of the joint, not just the pain.
The best injection for your knee arthritis comes down to your specific goals and symptoms. There's no single "best" option—only the right one for your situation. To make it clearer, here’s a breakdown of how they stack up.
| Injection Type | Mechanism of Action | Onset of Relief | Typical Duration | Ideal Candidate |
|---|---|---|---|---|
| Corticosteroids | Potent anti-inflammatory | Fast (1-3 days) | Short-term (1-3 months) | Someone with a severe, acute pain flare-up needing rapid relief. |
| Hyaluronic Acid | Joint lubrication and cushioning | Slow (several weeks) | Mid-term (up to 6 months) | A patient with chronic, moderate pain and stiffness during daily activities. |
| Platelet-Rich Plasma | Stimulates natural healing | Very slow (4-12 weeks) | Long-term (6-12+ months) | An individual with mild to moderate arthritis seeking a biological treatment. |
Ultimately, choosing an injection is a conversation you should have with your doctor. By talking through your pain patterns, activity level, and what you hope to achieve, you can land on the treatment that gives you the best shot at relief.
When you've tried all the conservative routes—the therapies, the injections, the lifestyle changes—and the knee pain still dictates your life, the conversation inevitably turns to surgery. For someone with end-stage, bone-on-bone arthritis, a total knee replacement isn't just a last resort; it's often the most reliable way to get back to a life without constant pain.
Making the call to have surgery is a massive decision, and it’s about so much more than what an X-ray shows. Sure, the film might show a joint with no cartilage left, but the real green light for surgery is when that damage completely hijacks your daily life. It’s a quality-of-life decision, plain and simple.
The perfect candidate for a total knee replacement is someone whose world has shrunk because of their knee. We're talking about people who can't make it through the grocery store, dread the stairs, or haven't had a good night's sleep in months because the pain is just relentless.
So, how do you know it's time? The biggest sign is when the less invasive treatments have stopped working. If you've given physical therapy a real shot, managed your weight, and tried injections without getting any lasting relief, surgery becomes the next logical step.
Another key indicator is when your mobility and independence are circling the drain. When your knee stops you from doing things you love, or even just getting through your day, it's a clear signal that the joint is doing more harm than good to your overall well-being.
The decision to go through with a knee replacement is deeply personal. You get there when the daily grind of living with arthritis pain becomes a heavier burden than the commitment of surgery and rehab.
Think of it this way: if you find yourself planning your day around how little you have to walk, or you’ve given up gardening because you just can't kneel anymore, you're a strong candidate. Your life has been so compromised that the benefits of a new knee far outweigh the risks and the tough recovery period ahead.
For the right person, a total knee replacement is one of the most successful procedures in modern medicine. It's designed to do two things really well: get rid of the arthritis pain and give you back a functional, stable joint. For many, this procedure is hands-down the best treatment for knee arthritis once all other avenues are closed.
The numbers back this up. Major studies consistently show that over 80% of patients are happy with their results, reporting huge improvements in both pain and function within a year. But it’s crucial to have realistic expectations. The goal is to eliminate that deep, arthritic ache, but a replaced knee will never feel exactly like the one you were born with.
Recovery is not a passive process. It demands a serious commitment from you.
The longevity of modern implants is also quite impressive. It’s interesting how fixing one major joint can have a positive ripple effect on your whole body, much like how a bad spinal disc can cause problems down your leg. Once the knee pain is gone, people get more active, which is great for everything from their heart to their spine. To see how interconnected these issues can be, you can explore our guide on degenerative disc disease treatment options.
Today's knee replacements are built to last. Medical registries show that revision rates—meaning the need for a do-over surgery—are only around 5–10% at the 10-to-15-year mark for many patient groups. You can read more about the effectiveness and longevity of TKA from clinical studies. For most people, this is a durable, long-term fix.
Trying to navigate all the options for knee arthritis can feel overwhelming. With so many choices, the real question isn't "what's the best treatment?" but rather, "what's the best treatment for my knee?" The answer always comes down to a personalized strategy, one that’s built around your specific situation, your goals, and just how bad your arthritis has become.
This isn't about jumping straight to the most aggressive option. In fact, the smartest approach is to climb what we call the "treatment ladder." You always start on the bottom rung with the least invasive, lowest-risk strategies. You only move up to the next step—like injections or surgery—when the foundational work isn't giving you the relief you need to live your life.
Your plan starts with a simple but critical conversation with your doctor to pin down two things: the current stage of your arthritis and what you honestly want to get back to doing.
The right plan is impossible without a clear-eyed look at where you are right now. Arthritis isn't just one thing; it's a spectrum.
Your personal goals are just as crucial as the diagnosis. Is your dream to get back on the tennis court, or is it just to make it through the grocery store without wincing in pain? Being specific with your doctor is key, as it will shape every decision you make together.
So what does this look like in the real world? A plan for a 55-year-old with moderate arthritis is going to be completely different from one for a 75-year-old with debilitating, end-stage disease.
Scenario 1: The Active 55-Year-Old with Moderate Arthritis
Let's imagine Sarah, a 55-year-old who loves to garden but is finding her moderate knee arthritis makes it tough to kneel and stand back up. Her goal is to manage the pain so she can stay active in her garden and take her dog for long walks.
Her personalized plan would start right at the bottom of the ladder:
Scenario 2: The 75-Year-Old with Severe Pain
Now, let's think about Robert. He's 75, and his advanced arthritis causes constant pain that wakes him up at night. He can barely make it to his mailbox. His goal is simple but profound: he just wants to walk without agonizing pain and get his independence back.
Robert has already tried everything on the lower rungs of the ladder. He’s done physical therapy, lost weight, and had multiple injections that don't help much anymore.
For patients like Robert, whose quality of life is severely compromised and for whom conservative treatments have failed, surgery is no longer a last resort—it becomes the most direct path to achieving their goals.
His personalized plan is at the very top of the ladder. He is a prime candidate for a total knee replacement because it offers the most predictable and definitive solution to his debilitating pain.
This decision-tree flowchart gives you a visual walk-through of the key checkpoints that often lead to a surgical consultation.
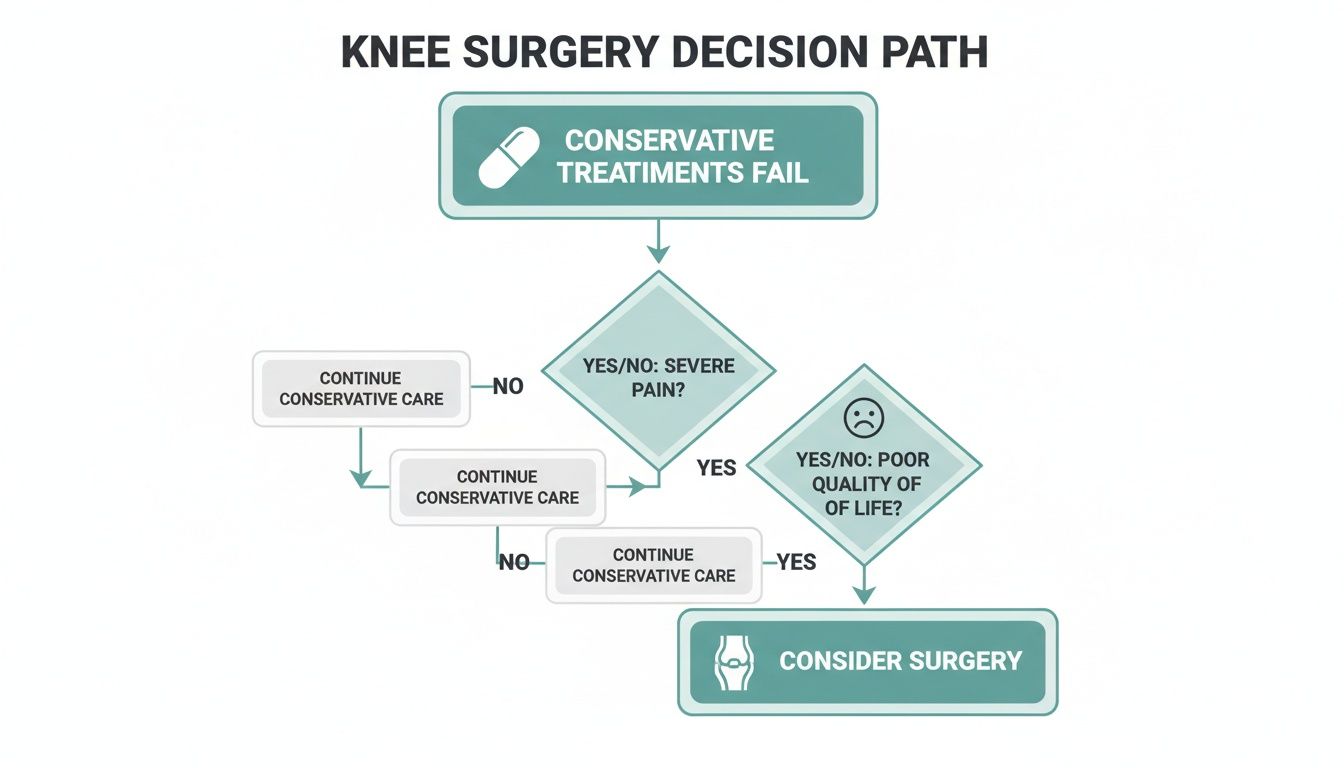
The flowchart makes it clear that the journey to surgery is a process of elimination. When conservative care fails to provide relief, and that failure is combined with severe pain and a poor quality of life, a definitive surgical solution often becomes the most logical next step. By working closely with your healthcare provider and moving up the treatment ladder methodically, you can build a plan that is perfectly suited to your knee, your body, and your life.
When you're dealing with knee arthritis, a lot of questions come up. It's natural to wonder what the best path forward is, not just for your knee, but for your life. Below, I’ve answered some of the most common questions I hear from patients, hoping to give you some clarity and confidence as you navigate your options.
Think of this as a starting point for a deeper conversation with your healthcare provider. The more you know, the more you can be an active partner in your own care.
Finding the right treatment isn't about picking one thing off a list; it's about building a strategy that fits you perfectly. A good specialist will act like a detective, piecing together clues about your specific situation to recommend the best approach.
Here’s what we look at together:
The most powerful treatment plans are rarely a single "fix." They're usually a smart combination of approaches that we adjust and adapt as your condition changes over time.
Yes, absolutely. For a huge number of people, surgery is not a foregone conclusion. The real secret to avoiding or at least significantly delaying a knee replacement is to be proactive with non-surgical strategies. I've seen many patients manage their symptoms successfully for years—sometimes for a lifetime—without ever needing to go under the knife.
The key is commitment. Success hinges on embracing conservative care and sticking with it. This means making real lifestyle changes, like maintaining a healthy weight to take the pressure off your joints and doing regular, low-impact exercise to build up the muscles that act as your knee's support system. A structured physical therapy program is also a game-changer, as it can fix the subtle biomechanical issues that put extra strain on the joint.
And when those core strategies aren't quite enough, advanced non-surgical options like injections or specialized chiropractic techniques can step in to provide major relief and improved function, pushing the need for surgery even further down the road.
This is the big question, and the answer really depends on the path you take. Some treatments provide quick, temporary relief, while others are a slow burn that leads to lasting change.
While there are many things you can do to manage knee arthritis, two lifestyle changes consistently punch way above their weight class. If you're going to focus your energy somewhere, start here.
The first is weight management. Every step you take sends a multiplied force of your body weight through your knees. Research shows that losing even a small amount—just 5-10% of your body weight—can slash the load on your knee joints, leading to a huge reduction in pain and slowing down cartilage damage.
The second is targeted exercise. You want to build a natural brace for your knee, and you do that by strengthening the muscles around it, especially your quadriceps and glutes. Strong muscles are like shock absorbers, shielding the joint from impact and making you more stable on your feet. It's one of the most important things you can do for the long-term health of your joint.
At Bonesetters Critical Chiropractic, we specialize in creating non-surgical game plans that get to the root cause of your knee pain. Dr. Leonard Hayes and our team use proven techniques like knee decompression and Class IV laser therapy to help you find relief that lasts, so you can get back to your life without surgery. Discover a truly personalized approach to your knee health by visiting us at https://bonesetters.org.