
When sciatica flares up, your first move is to find a position that takes the pressure off that pinched nerve. Lying on your back with pillows propping up your knees is a great start. For the first 48 hours, you'll want to use cold therapy to knock down the inflammation, then you can switch over to heat therapy to help those tight, angry muscles relax. These are your foundational, at-home first-aid steps.

When that tell-tale, shooting sciatic pain hits, the only thing on your mind is making it stop. Right now. In these first crucial hours, the goal isn't to launch into a complicated rehab program; it's about calming everything down. This is your immediate action plan to get some control back.
Your very first step should be getting off your feet. This simple act takes the direct pressure off your lower back and the sciatic nerve, which can provide an instant sense of relief.
One of the best go-to positions is lying flat on your back. Try it on a firm surface—the floor with a yoga mat is perfect, but a supportive mattress works too. The key is to slide a couple of pillows under your knees. This slight bend flattens your lower back just enough to create more space for the nerves exiting your spine.
Lying on your side can also work wonders. Just be sure to lie on the side opposite your pain. Tuck a pillow between your knees to keep your hips and spine aligned. This little trick stops your top leg from rolling forward and twisting your low back, which is the last thing that aggravated nerve needs.
Whatever you do, try to avoid sinking into a deep, soft sofa. It might feel good for a minute, but that "C" shape your spine makes can actually increase disc pressure and make things much worse in the long run.
Pro Tip: Everyone is different, so you might need to experiment a bit. Some people get relief by lying on their stomach with a pillow placed under their hips. The goal is to find a position that noticeably reduces your pain, and then hang out there for a while.
Using temperature to your advantage is a game-changer for acute sciatica, but you have to get the timing right.
For the first 48 to 72 hours, your mission is to reduce inflammation. That means ice is your best friend.
The cold constricts blood vessels, which helps dial down the swelling and numbs that sharp pain. If you want to dive deeper, we have a whole guide on how to use gel ice packs correctly for at-home care.
Once you’re past that initial 72-hour window, you can bring in the heat. A heating pad or a warm bath helps relax the tight, spasming muscles that are probably protesting by now. Heat brings fresh blood flow to the area, delivering oxygen and nutrients to kickstart the healing process. Again, keep it to 15-20 minute sessions. Many people find that alternating between ice and heat at this stage gives them the best of both worlds.
We used to tell people to go on complete bed rest, but we now know that's one of the worst things you can do. Too much inactivity can make you even stiffer and more sore. The trick is to avoid anything strenuous while still encouraging some gentle movement.
I'm talking about micro-movements. While you're lying in your comfortable position, try to slowly rock your pelvis back and forth. Or, gently pull one knee toward your chest, stopping the moment you feel anything more than a light stretch.
You are not trying to push through pain here. The goal is simply to keep blood flowing and prevent your muscles from completely locking up. If any movement causes that sharp, shooting pain down your leg, back off immediately. This phase is all about calming the system down before you're ready for more active recovery.

Once the fire of acute sciatic pain starts to die down, the very idea of moving can be terrifying. I get it. But this is the exact moment when careful, intentional exercise becomes your best friend for not just relief, but for building a truly resilient back.
The secret is to start slow and listen to your body. Think of it as a conversation. Your goal is to find movements that release tension, not create more of it. Imagine your muscles and nerves as a tangled rope; the initial rest and ice helped loosen the biggest knots, but now we need gentle stretching to carefully untangle the rest. Pushing too hard, too fast, will only pull those knots tighter.
These first few movements are designed to be as gentle as possible, targeting the key muscles that often compress the sciatic nerve. Always do them on a soft but firm surface, like a yoga mat.
Knee-to-Opposite-Shoulder Stretch
This is one of the safest and most effective stretches you can do, especially when you're just starting out.
This simple move is fantastic because it gets right at the piriformis and gluteal muscles. When these get tight, they can physically press on the sciatic nerve.
Reclining Pigeon Pose
This is a much gentler take on the classic yoga pose, giving you a great hip-opening stretch without putting any stress on your lower back.
This pose is a lifesaver for targeting those deep hip rotator muscles that can really aggravate the nerve.
Here’s the most important rule I tell my patients: "Stretch to tension, not to pain." If you feel a sharp, shooting, or electric jolt down your leg, you've gone too far. Back off immediately to a point where you feel a gentle pull, and hold that. That’s the sweet spot for natural relief without causing a flare-up.
Flexibility is only half the battle. If your core is weak, your lower back is left vulnerable to the exact same forces that caused your sciatica in the first place. A strong core—meaning the muscles in your abdomen, back, and glutes—creates a natural "corset" that supports and stabilizes your spine.
This muscular support system takes the daily pressure off your spinal discs and joints, preventing the tiny, cumulative injuries that lead to nerve compression.
These exercises build strength without putting your spine in a risky position. The key here is slow, controlled movement. Quality over quantity, always.
Glute Bridges
This move wakes up and strengthens your glutes, which are absolutely critical for supporting your pelvis and taking the strain off your lower back.
Bird-Dog Pose
This is a fantastic exercise for building true core stability and balance. It challenges you to keep your spine neutral while your limbs are moving.
For many people, the root of the problem is a deep muscle called the piriformis. When it gets tight, it can directly irritate the sciatic nerve—a common issue better known as piriformis syndrome and its treatment. Many of the stretches here are designed to help with that specific problem.
Consistency beats intensity every single time. A short, 10-15 minute routine every day will do you far more good than one long, painful session once a week.
Here’s a sample flow you can try:
| Phase | Exercise/Stretch | Duration/Reps | Focus |
|---|---|---|---|
| Warm-Up | Pelvic Tilts | 10-15 gentle rocks | Gently waking up the lower back |
| Stretching | Knee-to-Opposite-Shoulder | 3 reps per side, 30s hold | Releasing glute and piriformis tension |
| Stretching | Reclining Pigeon Pose | 3 reps per side, 30s hold | Deeply stretching the hip rotators |
| Strengthening | Glute Bridges | 2 sets of 12 reps | Activating and building glute support |
| Strengthening | Bird-Dog Pose | 2 sets of 10 reps/side | Improving core stability and balance |
This blend of stretching and strengthening is your roadmap—not just to get out of pain, but to build a more resilient back for the long haul. By investing this small amount of time each day, you are actively creating a body that can handle life's stresses, dramatically cutting your risk of future sciatica flare-ups.
Lasting relief from sciatica isn't something you find in a 15-minute stretching session. It’s built, moment by moment, in the way you live your life. The real key to moving past temporary fixes and toward genuine, long-term prevention is to address the small, daily habits that are quietly contributing to the problem.
This means taking an honest look at how you sit, stand, move, and even sleep. By making a few smart, powerful tweaks to these everyday routines, you can create an environment where your spine is supported and that angry sciatic nerve finally gets a chance to calm down.
For a lot of us, our workday is the main culprit behind sciatica flare-ups. Sitting for hours on end, especially in a chair that offers zero support, puts a massive amount of sustained pressure on your lower back. Over time, this constant compression can lead to the exact disc issues that irritate the sciatic nerve.
Think of an ergonomic workspace not as a perk, but as a fundamental part of keeping your spine healthy.
This awareness needs to extend beyond your desk, too. When you lift anything—a heavy box, a bag of groceries, your toddler—the golden rule is to bend at your knees and hips, never at your waist. Tighten your core muscles and let your powerful leg muscles do the work, keeping your back straight. It feels awkward at first, but this one habit shift takes a huge load off the vulnerable discs in your lower back.
Those hours you spend in bed are your body’s prime time for healing and recovery. But if you’re sleeping in the wrong position, you can easily undo all the progress you made during the day. If you consistently wake up feeling stiff and sore, your sleep setup is almost certainly part of the problem. Your goal is to keep your spine in a neutral, relaxed line all night long.
A supportive mattress is the foundation, but strategic pillow placement is the real secret weapon for getting sciatic nerve relief while you sleep. The right support can dramatically reduce nighttime pain and that dreaded morning stiffness.
If you’re a side sleeper, placing a firm pillow between your knees is non-negotiable. This simple trick stops your top leg from sliding forward and twisting your pelvis and lower back into an irritating position. For back sleepers, a pillow tucked under your knees works wonders by helping to maintain the natural, gentle curve of your lumbar spine, which reduces strain.
Stomach sleeping? It's honestly the worst position for anyone with back pain. It flattens your spine's natural curve and forces you to wrench your neck to one side for hours. If you absolutely cannot sleep any other way, try placing a flat pillow under your pelvis to help lessen some of that strain.
The weight you carry has a direct, mechanical effect on your spine. Every extra pound adds strain to the muscles and ligaments that support your lower back. The numbers are pretty stark: for every one pound of weight you lose, you relieve four pounds of pressure from your spinal joints. Getting to a healthy weight is one of the most impactful things you can do for long-term sciatica prevention.
What you put on your plate plays a massive role, too. Widespread inflammation in your body can make your nerves hypersensitive and your muscles feel tight and achy. An anti-inflammatory diet is all about choosing whole, unprocessed foods that help cool that internal fire.
Think of it like this: your diet can either fan the flames of inflammation or help put them out. By filling your plate with nutrient-dense foods, you’re not just helping manage your weight—you’re actively creating an internal environment that supports nerve health and dials down pain from the inside out.
While your own efforts with stretching and lifestyle changes are the bedrock of recovery, sometimes you hit a wall. That’s when bringing in a professional for some hands-on help can make a world of difference, especially for stubborn sciatica. These therapies go beyond what you can do at home, targeting the deep mechanical and muscular issues that keep that nerve aggravated.
Think of it like this: your daily exercises are like regular maintenance on your car. But when something is really stuck or out of alignment, you need a skilled mechanic. These therapies are that targeted tune-up for your body, designed to release deep tension, improve how your spine moves, and calm down that frazzled nervous system.
Deep tissue massage is a game-changer for the muscular side of sciatica. A good therapist knows how to hunt down the real culprits—often the piriformis and other deep gluteal muscles that can physically clamp down on the sciatic nerve. This isn't your average spa treatment; it's a focused effort to break up trigger points and adhesions that are causing nerve irritation.
Chiropractic care, on the other hand, zeroes in on the structural alignment of your spine. Using precise, gentle adjustments, a chiropractor can restore proper movement to spinal joints that have become stiff or misaligned. This often creates more space for the nerve roots, taking direct pressure off them. It’s not uncommon for patients to feel that sharp, shooting pain ease up significantly after just a few sessions.
Expert Tip: The one-two punch of massage (for muscles) and chiropractic care (for joints) is often the most effective approach. When your joints are moving freely, your muscles are less likely to spasm. And when your muscles are relaxed, your spinal alignment holds better. It's a powerful synergy.
Many of these hands-on techniques fall under the umbrella of manual therapy. You can learn more about how practitioners target the body's connective tissue by exploring methods like myofascial release.
Acupuncture takes a totally different, yet often incredibly effective, path to quieting nerve pain. This ancient practice uses ultra-thin needles inserted at specific points to modulate pain signals and stimulate your body’s own healing mechanisms.
If you’re skeptical, the science is starting to catch up. A comprehensive review of 11 different studies found that acupuncture was actually more effective at relieving sciatica pain than conventional drug therapies. You can read the full research about these findings for yourself. On a practical level, acupuncture helps your body release endorphins (its natural painkillers) and can reduce inflammation right at the source of the nerve irritation.
Practices like yoga and tai chi are brilliant because they work on two levels at once. They build physical strength and flexibility in the muscles supporting your spine, while also training your brain to better manage the sensation of pain.
This infographic really drives home the long-term principles of prevention, all of which are supported and enhanced by these complementary therapies.
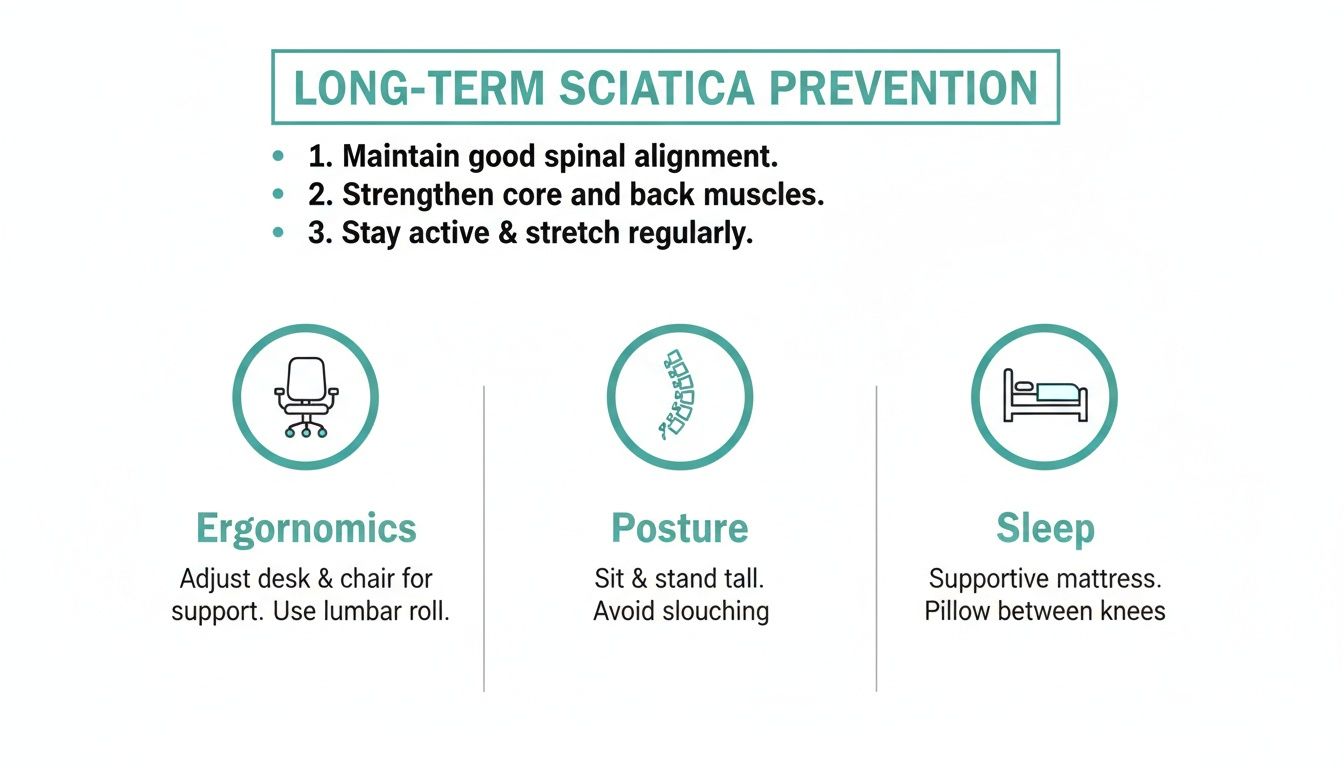
By dialing in your daily ergonomics, posture, and sleep habits, you build a solid foundation that helps these professional therapies deliver more lasting results.
When considering a therapy, it's crucial to find a licensed, experienced practitioner who has a track record of treating sciatica. Don't be shy—ask them about their approach and what you can realistically expect. For many people, adding one or more of these complementary treatments is the missing piece of the puzzle for finding lasting, natural relief.
What you eat has a direct, powerful impact on your body's inflammation levels—and inflammation is a major driver of sciatica pain. By choosing the right foods, you can help calm your system from the inside out, creating an environment that supports nerve healing instead of constant irritation.
Think of your diet as a foundational tool for managing pain. An anti-inflammatory eating plan gives your body the raw materials it needs to reduce swelling and support proper nerve function. This isn't about a restrictive, short-term diet; it's about making smart, consistent choices that build up over time.
Certain foods are absolute powerhouses when it comes to fighting inflammation. Weaving these into your regular meals can genuinely make a difference in your pain levels.
A fantastic place to start is with fatty fish like salmon, mackerel, and sardines. These are packed with omega-3 fatty acids, which are famous for their potent anti-inflammatory effects.
Beyond fish, try to load your plate with a rainbow of colorful fruits and vegetables.
Shifting your diet is a long-term strategy. You probably won't feel relief overnight, but consistently fueling your body with anti-inflammatory foods can gradually lower your baseline pain and reduce how often flare-ups happen.
While a food-first approach is best, some supplements can offer a more concentrated dose of support for nerve pain and inflammation. Just remember, this is an area where professional guidance is non-negotiable.
Vitamins from the B-complex family are crucial for nerve health. Vitamins B1, B6, and B12, in particular, are vital for maintaining the protective myelin sheath around your nerves and supporting proper signaling. A deficiency in any of these can sometimes be a contributing factor to nerve-related pain.
Herbal remedies also have a long history of use. Certain herbal and nutritional supplements have been traditionally used as natural treatments for sciatica by targeting pain and supporting the nerves, though scientific evidence varies. Potent anti-inflammatory herbs like turmeric, devil's claw, willow bark, and boswellia contain active compounds thought to reduce the inflammatory processes that can aggravate the sciatic nerve.
Before you even think about starting a new supplement, have a conversation with your healthcare provider. They can help you figure out the right dosage and, most importantly, make sure it won’t interfere with any other medications you’re taking. This is the only way to use supplements safely and effectively as part of your overall sciatica relief plan.
When you're dealing with the misery of sciatica, a million questions can run through your mind. Getting straight answers from someone who's been there can help you feel more in control of your recovery. Let’s clear up some of the most common things people ask.
This is always the first question, and the honest-to-goodness answer is, "it really depends." If you're dealing with a sudden flare-up from something simple like a muscle strain, you could feel a world of difference in just a few days or a couple of weeks by diligently using ice, gentle stretches, and smart positioning.
But if the root cause is something more significant—say, a herniated disc or spinal stenosis—the road is a bit longer. You'll need to be patient. For these deeper issues, you're realistically looking at four to six weeks of consistent, daily effort before you'll notice a real, lasting shift. It’s not about finding a magic bullet; it's about systematically calming the inflammation and rebuilding your body's support system.
Absolutely not. Let's be crystal clear on this: there’s a massive difference between the mild discomfort of a good stretch and that sharp, zinging, electrical pain that defines a sciatica flare-up. Forcing your way through true nerve pain is counterproductive. It will only anger the nerve further and can seriously derail your progress.
Listen to Your Body's Warning Signal: If any movement or exercise makes the pain worse, sends it further down your leg, or turns a dull ache into a sharp jab—stop. Immediately. The whole point of these exercises is to create space and relief, not to provoke the nerve.
Think of that pain as your body's alarm system. It's telling you to back off.
The old advice was to hole up in bed for days, but we now know that’s a mistake. While the instinct is to stay completely still, more than a day or two of total rest can actually make things worse. Your muscles get weak and stiff, which only prolongs the problem.
The trick is finding the right balance.
We call this approach "active recovery." You're dialing back your activity level, not shutting it down entirely. This keeps nourishing blood flowing to the injured area and prevents the surrounding muscles from seizing up, which is exactly what you need to heal.
At Bonesetters Critical Chiropractic, we focus on pinpointing the true source of your sciatica to deliver relief that lasts, without resorting to surgery. If you've tried everything at home and still feel stuck, discover how our evidence-based chiropractic care can help you reclaim a pain-free life.